Asociación entre metabolismo mineral e infección por virus de Hepatitis C en pacientes con enfermedad renal crónica en hemodiálisis.
Resumen
Introducción: Epidemiológicamente se ha reportado que los pacientes con infección crónica por el Virus de Hepatitis C (VHC), podrían presentar alteraciones en el metabolismo mineral óseo. Objetivo: Evaluar la relación entre la infección VHC y el metabolismo mineral en pacientes con enfermedad renal crónica en hemodiálisis. Materiales y Métodos: Estudio tipo corte transversal, caso-control, comparativo. La muestra, no aleatorizada, fue de 1213 paciente con diagnóstico serológico positivo para VHC (casos) y 2933 pacientes con serología negativa hepatitis C (controles) de ambos sexos, con edad de 18-80 años. Los biomarcadores séricos de metabolismo mineral (PTH, vitamina D, calcio, fósforo, magnesio, hierro), funcionalismo hepático y la serología para virus de VHA, VHB, VH, VIH y sífilis fueron determinados en ayunas, en periodo inter-diálisis. Resultados: La edad promedio de la muestra evaluada fue 53,16 ± 15.45 años (IC955% de 52,69 a 53, 64 años). En los casos, el promedio de las concentraciones séricas de: fósforo, magnesio, hierro, ferritina y parathormona; así como las actividades enzimáticas séricas de AST, ALT y ALP; y de los índices FIB4y APRI fueron significativamente mayores a los del grupo control. (Prueba t-Student, p< 0.01, alfa 0.05). La frecuencia de hiperparatiroidismo secundario severo (PTH intacta sérica mayor de 600 pg/ml) y de insuficiencia de vitamina D en los casos (n = 544/1213 y n = 478/1213, respectivamente), fue significativamente mayor que la observada en los controles (n = 834/2933, y n = 830/2933, p<0,0001; prueba Chi- cuadrado; alfa 0,05). Conclusión: La infección con HVC en pacientes con ERC en hemodiálisis se asocia con mayor frecuencia de hiperparatiroidismo secundario severo e insuficiencia de Vitamina D, determinada por una concentración sérica mayor de PTH intacta y menor de vitamina D.
ESCUCHE EL RESUMEN HANCIENDO CLIC EN EL IDIOMA DE SU PREFERENCIA:
EspañolEnglish
Portugues
Japones
Palabras clave
Texto completo:
PDFReferencias
Levey AS, Eckardt KU, Dorman NM, et al. Nomenclature for kidney function and disease: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int. 2020;97:1117-29.
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98(4S):S1-115.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105:S1-197.
Bello AK, Okpechi IG, Levin A, et al. An update on the global disparities in kidney disease burden and care across world countries and regions. Lancet Glob Health. 2024;12:e382-95.
World Health Organization. Hepatitis C [Internet]. Geneva: WHO; 2025 [cited 2025 Sep 22]. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-c
Kenfack-Momo R, Ngounoue MD, Kenmoe S, et al. Global epidemiology of hepatitis C virus in dialysis patients: a systematic review and meta-analysis. PLoS One. 2024;19:e0284169.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD). Kidney Int Suppl (2011). 2017;7(1):1-59.
Backstedt D, Pedersen M, Choi M, Seetharam A. 25-Vitamin D levels in chronic hepatitis C infection: association with cirrhosis and sustained virologic response. Ann Gastroenterol. 2017;30:344-8.
Gabr SA, Alghadir AH. Handgrip strength and vitamin D as predictors of liver fibrosis and malnutrition in chronic hepatitis C patients. Dis Markers. 2021;2021:6665893.
Bellorin-Font E, Carlini RG. Kidney disease in Venezuela: the impact of a lingering humanitarian crisis. Nat Rev Nephrol. 2021;17:507-8.
Martínez D, Papuzinski C, Stojanova J, Arancibia M. General concepts in biostatistics and clinical epidemiology: observational studies with case-control design. Medwave. 2019;19(10):e7716.
The Nuremberg Code (1947). BMJ. 1996;313:1448.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-4.
United Nations. International Covenant on Civil and Political Rights [Internet]. New York: UN; 1966 Disponible en: https://www.ohchr.org/en/instruments-mechanisms/ instruments/international-covenant-civil-and-political-rights
Vandenbroucke JP, von Elm E, Altman DG, et al; STROBE initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147(8):W163-94.
Fabrizi F, Dixit V, Messa P, Martin P. Hepatitis C-related liver disease in dialysis patients. Contrib Nephrol. 2012;176:42-53.
Mutlag F, Elaibi HK, Hasan AA. The effect of vitamin D and parathyroid on hepatitis C patients and non-hepatitis C patients on chronic hemodialysis. J Appl Microbiol Biochem. 2023;7(5):187.
Zhang M, Han Z, Lin Y, et al. Understanding the relationship between HCV infection and progression of kidney disease. Front Microbiol. 2024;15:1418301.
Gómez-Gutiérrez C, Chávez-Tapia NC, Ponciano-Rodríguez G, Uribe M, Méndez-Sánchez N. Prevalence of hepatitis C virus infection among patients undergoing haemodialysis in Latin America. Ann Hepatol. 2015;14:807-14.
Greeviroj P, et al. The world prevalence, associated risk factors and mortality of hepatitis C virus infection in hemodialysis patients: a meta-analysis. J Nephrol. 2022;35:2269-82.
Salari N, et al. Global prevalence of hepatitis C in general population: a systematic review and meta-analysis. Travel Med Infect Dis. 2022;46:102255.
Nguyen DB, et al. A large outbreak of hepatitis C virus infections in a hemodialysis clinic. Infect Control Hosp Epidemiol. 2016;37:125-33.
Platt L, et al. Prevalence and burden of HCV co-infection in people living with HIV: a global systematic review and meta-analysis. Lancet Infect Dis. 2016;16:797-808.
Jin F, et al. Prevalence and incidence of hepatitis C virus infection in men who have sex with men: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:39-56.
Salari N, et al. Global prevalence of hepatitis C in prisoners: a comprehensive systematic review and meta-analysis. Arch Virol. 2022;167:1025-39.
Corcoran GD, et al. Hepatitis C virus infection in haemodialysis patients: a clinical and virological study. J Infect. 1994;28:279-85.
Shimokura G, et al. Patient-care practices associated with an increased prevalence of hepatitis C virus infection among chronic hemodialysis patients. Infect Control Hosp Epidemiol. 2011;32:415-24.
Kasraian L, et al. The prevalence of hepatitis C infection in blood donors: a meta-analysis and systematic review. Iran Red Crescent Med J. 2020;22(1):e102568.
Pujol FH, Ponce JG, Lema MG, et al. High incidence of hepatitis C virus infection in hemodialysis patients in units with high prevalence. J Clin Microbiol. 1996;34:1633-6.
Rosa-Diez G, Gonzalez-Bedat M, Pecoits-Filho R, et al. Renal replacement therapy in Latin American end-stage renal disease. Clin Kidney J. 2014;7:431-6.
Saxena AK, Panhotra BR. The vulnerability of middle-aged and elderly patients to hepatitis C virus infection in a high-prevalence hospital-based hemodialysis setting. J Am Geriatr Soc. 2004;52:242-6.
Tajbakhsh R. Prevalence of hepatitis C and B virus infections among hemodialysis patients in Karaj, Iran. Saudi J Kidney Dis Transpl. 2015;26:792-6.
Al-Jamal M, Al-Qudah A, Al-Shishi KF, et al. Hepatitis C virus infection in hemodialysis patients in the south of Jordan. Saudi J Kidney Dis Transpl. 2009;20:488-92.
Stehman-Breen CO, Emerson S, Gretch D, Johnson RJ. Risk of death among chronic dialysis patients infected with hepatitis C virus. Am J Kidney Dis. 1998;32:629-34.
Kwon E, Cho JH, Jang HM, et al; Clinical Research Center for End Stage Renal Disease (CRC for ESRD) Investigators. Differential effect of viral hepatitis infection on mortality among Korean maintenance dialysis patients: a prospective multicenter cohort study. PLoS One. 2015;10:e0135476.
Rogal SS, Yan P, Rimland D, et al; Electronically Retrieved Cohort of HCV Infected Veterans Study Group. Incidence and progression of chronic kidney disease after hepatitis C seroconversion: results from ERCHIVES. Dig Dis Sci. 2016;61:930-6.
Fabrizi F, Verdesca S, Messa P, Martin P. Hepatitis C virus infection increases the risk of developing chronic kidney disease: a systematic review and meta-analysis. Dig Dis Sci. 2015;60:3801-13.
Fabrizi F, Donato FM, Messa P. Hepatitis C and its metabolic complications in kidney disease. Ann Hepatol. 2017;16:851-8.
Henson JB, Sise ME. The association of hepatitis C infection with the onset of CKD and progression into ESRD. Semin Dial. 2019;32:108-18.
Marinaki S, Boletis JN, Sakellariou S, Delladetsima IK. Hepatitis C in hemodialysis patients. World J Hepatol. 2015;7:548-58.
Angelini C, Badalamenti S, Lunghi G, et al. Evidence against hepatitis C virus trapping in dialysis membranes. Nephrol Dial Transplant. 2002;17:317-8.
Fabrizi F, Lunghi G, Finazzi S, et al. Decreased serum aminotransferase activity in patients with chronic renal failure: impact on the detection of viral hepatitis. Am J Kidney Dis. 2001;38:1009-15.
Yasuda K, Okuda K, Endo N, et al. Hypoaminotransferasemia in patients undergoing long-term hemodialysis: clinical and biochemical appraisal. Gastroenterology. 1995;109:1295-303.
Arrayhani M, Sqalli T, Tazi N, et al. Noninvasive assessment of liver fibrosis in chronic hemodialysis patients with viral hepatitis C. Pan Afr Med J. 2015;22:273.
Schiavon L, Schiavon JL, Carvalho Filho RJ, et al. Simple blood tests as noninvasive markers of liver fibrosis in hemodialysis patients with chronic hepatitis C virus infection. Hepatology. 2007;46:307-14.
Chen HL, Cheng CL, Chun JL, et al. The ratio of aminotransferase to platelets is a useful index for predicting hepatic fibrosis in hemodialysis patients with chronic hepatitis C. Kidney Int. 2010;78:103-9.
Carvalho-Filho RJ, Feldner AC, Silva AE, Ferraz ML. Management of hepatitis C in patients with chronic kidney disease. World J Gastroenterol. 2015;21:408-22.
Schiavon LL, Schiavon JL, Filho RJ, et al. Simple blood tests as noninvasive markers of liver fibrosis in hemodialysis patients with chronic hepatitis C virus infection. Hepatology. 2007;46:307-14.
Pestana NF, Equi CMA, Gomes CP, et al. Aminotransferase-to-platelet ratio index and Fibrosis-4 index score predict hepatic fibrosis evaluated by transient hepatic elastography in hepatitis C virus-infected hemodialysis patients. Eur J Gastroenterol Hepatol. 2021;33(Suppl 1):e260-5.
Ratiu IA, Mihaescu A, Olariu N, et al. Hepatitis C virus infection in hemodialysis patients in the era of direct-acting antiviral treatment: observational study and narrative review. Medicina (Kaunas). 2024;60:2093.
Bishop CW, Ashfaq A, Choe J, Sprague SM. Extended-release calcifediol normalized 1,25-dihydroxyvitamin D and prevented progression of secondary hyperparathyroidism in hemodialysis patients in a pilot randomized clinical trial. Am J Nephrol. 2025;56:1-11.
Pothula VV, Scialla JJ. Momentum toward patient outcome trials in chronic kidney disease-mineral bone disorder. Curr Opin Nephrol Hypertens. 2025;34(4):304-13.
Priyadarshini G, Parameswaran S, Sahoo J, et al. The vitamin D spectrum: insights into 25(OH)D and VDBP in chronic kidney disease and post-transplant. Sci Rep. 2025;15:18395.
DOI: http://dx.doi.org/10.61155/gen.v79i4.785
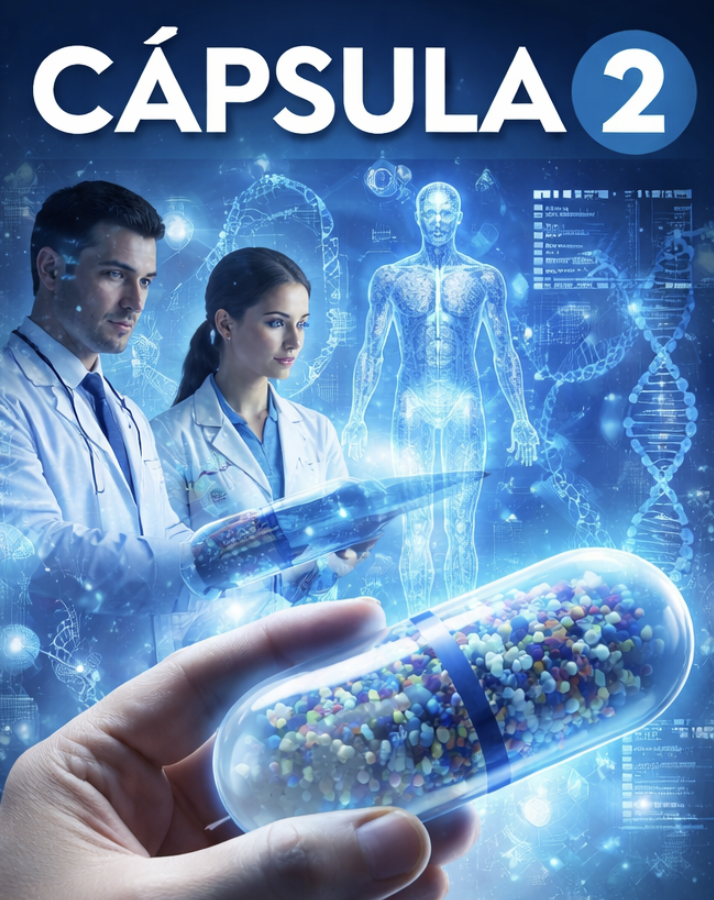
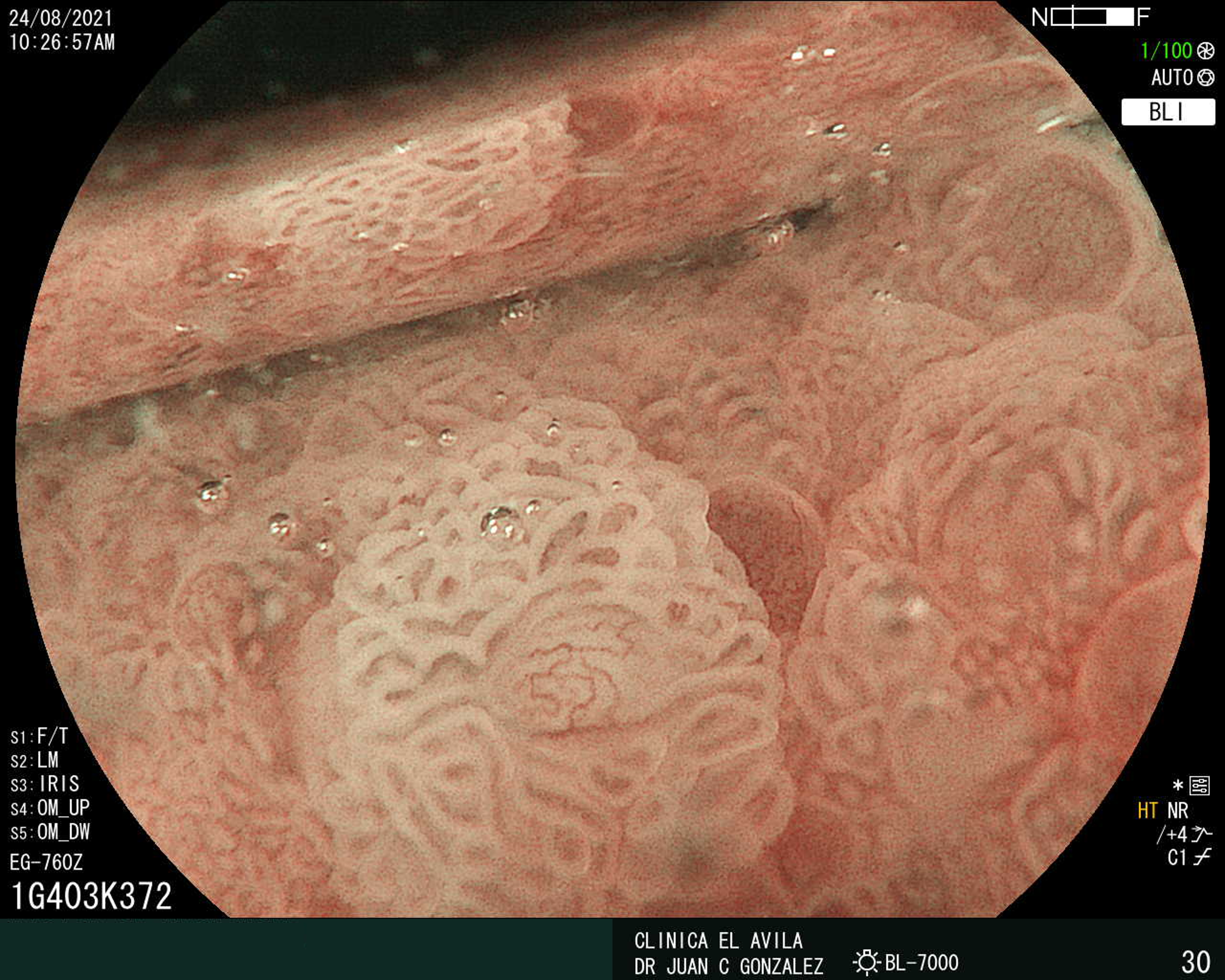
IMÁGENES GEN
| Figura 1. Tumor Neuroendocrino Gástrico | Figura 2. Hiperplasia de Células Neuroendocrinas en estómago |
 |  |
 |  |  |
ISSN: 0016-3503 e-ISSN: 2477-975X