Valor pronóstico de uricemia para enfermedad hepática grasa asociada a disfunción metabólica
Resumen
Introducción: Evidencia epidemiológica muestra la asociación entre Esteatosis Hepática Asociada a Disfunción Metabólica (EHADM) y elevación de la uricemia. Objetivo: Determinar valor pronóstico de la uricemia para EHADM. Métodos: Estudio epidemiológico de tipo corte transversal, caso-control. 47 sujetos de ambos sexos, con edad de 18-75 años, fueron clasificados según la presencia de EHADM (casos, n=24) o ausencia de EHADM (controles, NEHADM, n=23). Se evaluó: la concentración sérica de ácido úrico (Au) y biomarcadores para enfermedad metabólica, la fibrosis hepática por elastografía de onda de corte ultrasonográfica y el valor límite para uricemia asociada a EHADM con base en la curva característica del operador receptor. Resultados: La EHADM fue mayor en mujeres (55.26 % contra 33.33 % en hombres). La dislipidemia por HDL-colesterol (98%) y obesidad abdominal (76.59%) fueron los factores de riesgo más frecuentes para EHADM. La EHADM se correlacionó positivamente con el diámetro longitudinal de lóbulo hepático derecho (LHD) y el índice HOMA (p =0.006); uricemia y Au/HDLc (p = 0.0001). El promedio de uricemia en EHADM (7,49±1,82 mg/dl; IC95% 6,76- 8,21 mg/dL), fue mayor que en NEHDAM (5,37±1,06 mg/dl; IC95% 4.94-5.80 mg/dL, p = 0.0001, prueba t de Student, alfa = 0.05). El valor límite para uricemia asociada a EHADM fue de 6.02 mg/dL (sensibilidad 70.83%; especificidad 82.61%; VPP 80.95% y VPN 73.08%, RR 3.01); y para LHD de 13.15 cm (sensibilidad 62.50%; especificidad 73.91%; VPP 71.43% y VPN 65.38 %, RR 2.06). Conclusión: Se muestran valores límites de uricemia y de la longitud del lóbulo hepático derecho asociados a EHADM.
ESCUCHE EL RESUMEN HANCIENDO CLIC EN EL IDIOMA DE SU PREFERENCIA:
Español
English
Portugues
Palabras clave
Texto completo:
PDFReferencias
Ayonrinde OT. Historical narrative from fatty liver in the nineteenth century to contemporary NAFLD - Reconciling the present with the past. JHEP Rep. 2021;3(3): 100261.
Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158(7): 1999-2014.e1.
Wang D, Xu Y, Zhu Z, Li Y, Li X, Li Y, et al. Changes in the global, regional, and national burdens of NAFLD from 1990 to 2019: A systematic analysis of the global burden of disease study 2019. Front. Nutr. 2022; 9: 1047129.
Ge X, Zheng L, Wang M, Du Y, Jiang J. Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990–2017: a population based observational study. BMJ Open. 2020;10(8): e036663.
Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022; 133: 155217.
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019; 15(5): 288-298.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017; 390(10113): 2627-42.
GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023; 402(10397):203-234. Erratum in: Lancet. 2023; 402(10408): 1132.
Zhang J, Huang X, Dong L, Yang Y, Kong D. Epidemiology of lean/non-obese nonalcoholic fatty liver disease in China: A systematic review and meta-analysis. Saudi Med J. 2023;44(9):848-863.
Shi Y, Wang Q, Sun Y, Zhao X, Kong Y, Ou X et al. The Prevalence of Lean/Nonobese Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. J Clin Gastroenterol. 2020; 54(4):378-387.
Kanwal F, Shubrook JH, Younossi Z, Natarajan Y, Bugianesi E, Rinella ME et al. Preparing for the NASH Epidemic: A Call to Action. Gastroenterology. 2021;161(3):1030-1042.e8.
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11-20.
Rinella ME, Tacke F, Sanyal AJ, Anstee QM; participants of the AASLD/EASL Workshop. Report on the AASLD/EASL joint workshop on clinical trial endpoints in NAFLD. J Hepatol. 2019; 71(4): 823-833.
Neuberger J, Patel J, Caldwell H, Davies S, Hebditch V, Hollywood C et al. Guidelines on the use of liver biopsy in clinical practice from the British Society of Gastroenterology, the Royal College of Radiologists and the Royal College of Pathology. Gut. 2020; 69(8):1382-1403.
McGlinchey AJ, Govaere O, Geng D, Ratziu V, Allison M, Bousier J et al. Metabolic signatures across the full spectrum of non-alcoholic fatty liver disease. JHEP Rep. 2022;4(5):100477.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018; 67(1):328-357.
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M et al. New definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73(1):202-9.
Darmawan G, Hamijoyo L, Hasan I. Association between Serum Uric Acid and Non-Alcoholic Fatty Liver Disease: A Meta-Analysis. Acta Med Indones. 2017; 49(2):136-147.
Huang F, Liu A, Fang H, Geng X. Serum uric acid levels in non-alcoholic steatosis patients: a meta-analysis. Asia Pac J Clin Nutr. 2017; 26(2):334-42.
Zhou Y, Wei F, Fan Y. High serum uric acid and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. Clin Biochem. 2016; 49(7-8):636-42.
Jaruvongvanich V, Ahuja W, Wirunsawanya K, Wijarnpreecha K, Ungprasert P. Hyperuricemia is associated with nonalcoholic fatty liver disease activity score in patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017; 29(9): 1031-35.
Fernández Rodríguez CM, Aller R, Gutiérrez García ML, Ampuero J, Gómez-Camarero J, Martín-Mateos RMª et al. Higher levels of serum uric acid influences hepatic damage in patients with non-alcoholic fatty liver disease (NAFLD). Rev Esp Enferm Dig. 2019; 111(4): 264-69.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016; 64(1): 73-84.
Younossi ZM. Non-alcoholic fatty liver disease - A global public health perspective. J Hepatol. 2019; 70(3):531-44.
Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013; 10(6): 330-44.
González Gutiérrez R, Cedeño KA, Angulo AI, Moliné ME, Añez RJ, Salazar JJ et al. Hiperuricemia como factor de riesgo para obesidad en adultos de la ciudad de Maracay, Venezuela. Revista Latinoamericana de Hipertensión. 2015: 10(1):08-14.
Ruiz-Fernández N; Nobrega, D. Índice de hígado graso en mujeres adultas del estado Carabobo, Venezuela. Asociación con síndrome metabólico y riesgo cardiometabólico. Acta Bioclínica. 2021; 11(22); 69-93.
Pontiles de Sánchez M, Morón de Salim A, Rodríguez de Perdomo H, Perdomo Oramas G. Prevalencia de la enfermedad de higado graso no alcohólico (EHGNA) en una población de niños obesos en Valencia, Venezuela. Arch Latinoam Nutr. 2014; 64(2): 73-82.
Camacho N, Guillén M, Molina Z, Zanchetti R, Paoli M, Cicchetti R et al. Esteatosis hepática en niños y adolescentes obesos: prevalencia y correlación con medidas antropométricas y niveles de lípido e insulina. Rev Venez Endocrinol Metab. 2010; 8:19-29.
Santomauro M, Paoli-Valeri M, Fernández M, Camacho N, Molina Z, Cicchetti R et al. Hígado graso no alcohólico y su asociación con variables clínicas y bioquímicas en niños y adolescentes obesos: efecto de un año de intervención en el estilo de vida. Endocrinol Nutr. 2012; 59(6):346-53.
Vaz K, Clayton-Chubb D, Majeed A, Lubel J, Simmons D, Kemp W et al. Current understanding and future perspectives on the impact of changing NAFLD to MAFLD on global epidemiology and clinical outcomes. Hepatol Int. 2023; 17(5):1082-1097.
Martínez D, Papuzinski C, Stojanova J, Arancibia M. General concepts in biostatistics and clinical epidemiology: observational studies with case-control design. Medwave. 2019;19(10): e7716
López-Alvarenga JC, Reding-Berrnal A, Pérez-Navarro M, Sobrino S. Cómo se puede estimar el tamaño de la muestra de un estudio. Dermatol Rev Mex 2010; 54(6): 375-79.
Duffau T. Gastón. Tamaño muestral en estudios biomédicos. Rev. chil. Pediatr. 1999; 70(4 ): 314-24.
Xie Y, Huang K, Zhang X, Wu Z, Wu Y, Chu J, et al.. Association of serum uric acid-to-high-density lipoprotein cholesterol ratio with non-alcoholic fatty liver disease in American adults: a population-based analysis. Front Med (Lausanne). 2023; 10: 1164096.
The Nuremberg Code (1947). BMJ 1996; 313:1448.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-94.
Pacto Internacional de Derechos Civiles y Políticos. https://www.ohchr.org/es/instruments-mechanisms/instruments/international-covenant-civil-and-political-rights.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. STROBE initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007; 147(8): W163-94.
Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al.. Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association. Hypertension. 2019; 73(5): e35-e66.
Dasarathy S, Dasarathy J, Khiyami A, Joseph R, Lopez R, McCullough AJ. Validity of real time ultrasound in the diagnosis of hepatic steatosis: a prospective study. J Hepatol 2009;51:1061-67
Bae JS, Lee DH, Suh KS, Kim H, Lee KB, Lee JY et al. Noninvasive assessment of hepatic steatosis using a pathologic reference standard: comparison of CT, MRI, and US-based techniques. Ultrasonography. 2022; 41(2): 344-54.
Hajian-Tilaki K. The choice of methods in determining the optimal cut-off value for quantitative diagnostic test evaluation. Stat Methods Med Res. 2018;27(8):2374-83.
Cerda J, Cifuentes L. Uso de curvas ROC en investigación clínica: Aspectos teórico-prácticos. Rev. chil. infectol. 2012;29 (2): 138-41.
Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E,, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2019; 69: 2672-82.
Hagström H, Vessby J, Ekstedt M, Shang Y. 99% of patients with NAFLD meet MASLD criteria and natural history is therefore identical. J Hepatol. 2024;80(2): e76-e77.
Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77(4):1335-1347.
Mahady SE, George J. Predicting the future burden of NAFLD and NASH. J Hepatol 2018; 69: 774–75.
Pimpin L, Cortez-Pinto H, Negro F, Corbould E, Lazarus JV, Webber L, et al. Burden of liver disease in Europe: epidemiology and analysis of risk factors to identify prevention policies. J Hepatol 2018;69: 718–35.
Rojas YAO, Cuellar CLV, Barron KMA, Verdugo JPA, Miranda AL. Non-alcoholic fatty liver disease prevalence in Latin America: a systematic review and meta-analysis. Ann Hepatol. 2022;18(3):528-35.
Pinto Marques Souza de Oliveira C, Pinchemel Cotrim H, Arrese M. Nonalcoholic fatty liver disease risk factors in Latin American populations: current scenario and perspectives. Clin Liver Dis (Hoboken). 2019;13(2):39-42.
Lopez-Velazquez JA, Silva-Vidal KV, Ponciano-Rodríguez G, Chávez-Tapia NC, Arrese M, Uribe M, Méndez-Sánchez N. The prevalence of nonalcoholic fatty liver disease in the Americas. Ann Hepatol. 2014; 13:166-78.
Ballering AV, Olde Hartman TC, Verheij R, Rosmalen JGM. Sex and gender differences in primary care help-seeking for common somatic symptoms: a longitudinal study. Scand J Prim Health Care. 2023;41(2):132-39.
Wang Y, Hunt K, Nazareth I, Freemantle N, Petersen I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open. 2013;3(8):e003320.
Nagral A, Bangar M, Menezes S, Bhatia S, Butt N, Ghosh J, et al. Gender Differences in Nonalcoholic Fatty Liver Disease. Euroasian J Hepatogastroenterol. 2022;12(Suppl 1):S19-S25.
Kojima S, Watanabe N, Numata M, et al. Increase in the prevalence of fatty liver in Japan over the past 12 years: analysis of clinical background. J Gastroenterol. 2003;38(10):954–61.
Zhou YJ, Li YY, Nie YQ, Ma JX, Lu LG, Shi SL et al. Prevalence of fatty liver disease and its risk factors in the population of South China. World J Gastroenterol. 2007;13(47):6419–24.
Pizzi La Veglia R, Parilli MF. Consenso Venezolano De Menopausia 2018. Consideraciones generales, Rev Obstet Ginecol Venez 2018;78(Supl 1): S4 - S12.
Castro-Martínez MG, Banderas-Lares DZ, Ramírez-Martínez JC, Escobedo-de la Peña J. Prevalence of nonalcoholic fatty liver disease in subjects with metabolic syndrome. Cir Cir. 2012 Mar-Apr;80(2):128-33.
Kontush A, de Faria EC, Chantepie S, Chapman MJ, A. Normotriglyceridemic, low hdl-cholesterol phenotype is characterised by elevated oxidative stress and hdl particles with attenuated antioxidative activity. Atherosclerosis. (2005) 182:277–85.
Huh Y, Nam GE, Lim J, Park HS. Trends in the high blood glucose and non-alcoholic fatty liver disease among Korean adolescents. Endocr J. 2022;69(11):1295-302.
Deng J, Han Z, Tang H, Yao C, Li X, Xu J et al. Elevated fasting glucose level increases the risk of fatty liver disease: a 10-year study of 31,154 individuals. BMC Gastroenterol. 2022;22(1):521.
Zou Y, Yu M, Sheng G. Association between fasting plasma glucose and nonalcoholic fatty liver disease in a nonobese Chinese population with normal blood lipid levels: a prospective cohort study. Lipids Health Dis. 2020;19(1):145.
Francque SMA, Dirinck E. NAFLD prevalence and severity in overweight and obese populations. Lancet Gastroenterol Hepatol. 2023;8(1):2-3.
Quek J, Chan KE, Wong ZY, Tan C, Tan B, Lim WH, et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8(1):20-30.
Zhang J, Xu Q, Lai F, Chen N, Lin M, Liu Y et al. Joint associations of metabolically healthy abdominal obesity and non-alcoholic fatty liver disease with prediabetes and diabetes in Chinese adults. BMJ Open Diab Res Care 2021; 9:e002362
Baffy G, Brunt EM, Caldwell SH. Hepatocellular carcinoma in non-alcoholic fatty liver disease: an emerging menace. J Hepatol. 2012;56(6):1384-91.
Park EJ, Lee JH, Yu GY, He G, Ali SR, Holzer RG, et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell. 2010;140(2):197-208.
Marengo A, Rosso C, Bugianesi E. Liver Cancer: Connections with Obesity, Fatty Liver, and Cirrhosis. Annu Rev Med. 2016; 67:103-17.
Zheng J, Zhao M, Li J, Lou G, Yuan Y, Bu S, Xi Y.. Obesity-associated digestive cancers: A review of mechanisms and interventions. Tumour Biol. 2017; 39(3):1010428317695020
Wijarnpreecha K, Panjawatanan P, Lekuthai N, Thongprayoon C, Cheungpasitporn W, Ungprasert P. Hyperuricaemia and risk of nonalcoholic fatty liver disease: A meta-analysis. Liver Int. 2017;37(6):906-918.
Jaruvongvanich V, Ahuja W, Wirunsawanya K, Wijarnpreecha K, Ungprasert P. Hyperuricemia is associated with nonalcoholic fatty liver disease activity score in patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017;29(9):1031-1035.
Jaruvongvanich V, Ahuja W, Wijarnpreecha K, Ungprasert P. Hyperuricemia is not associated with severity of liver fibrosis in patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017;29(6):694-697.
Toprak K, Yılmaz R, Kaplangoray M, Memioğlu T, İnanır M, Akyol S, et al. Comparison of the effect of uric acid/albumin ratio on coronary colleteral circulation with other inflammation-based markers in stable coronary artery disease patients. Perfusion. 2023:2676591231202105.
Kawamoto R, Kikuchi A, Ninomiya D, Tokumoto Y, Kumagi T. Serum uric acid to creatinine ratio is a useful predictor of all-cause mortality among hypertensive patients. Clin Hypertens. 2023;29(1):10.
Yu X, Sun F, Ming J, Liang S, Zhang W, Wang L, et al. Serum uric acid to high-density lipoprotein cholesterol ratio is a promising marker for identifying metabolic syndrome in nondiabetic Chinese men. Postgrad Med. 2023;135(7):741-749.
Wang R, Xue F, Wang L, Shi G, Qian G, Yang N, Chen X. Serum uric acid to creatinine ratio is associated with higher prevalence of NAFLD detected by FibroScan in the United States. J Clin Lab Anal. 2022;36(8):e24590.
Choi J, Joe H, Oh JE, Cho YJ, Shin HS, Heo NH.. The correlation between NAFLD and serum uric acid to serum creatinine ratio. PLoS One. 2023;18(7):e0288666
Xie Y, Huang K, Zhang X, Wu Z, Wu Y, Chu J. Association of serum uric acid-to-high-density lipoprotein cholesterol ratio with non-alcoholic fatty liver disease in American adults: a population-based analysis. Front Med (Lausanne). 2023;10:1164096.
Oral A, Sahin T, Turker F, Kocak E. Relationship Between Serum Uric Acid Levels and Nonalcoholic Fatty Liver Disease in Non-Obese Patients. Medicina (Kaunas). 2019;55(9):600.
Wei F, Li J, Chen C, Zhang K, Cao L, Wang X, et al. Higher Serum Uric Acid Level Predicts Non-alcoholic Fatty Liver Disease: A 4-Year Prospective Cohort Study. Front Endocrinol (Lausanne). 2020;11:179.
DOI: http://dx.doi.org/10.61155/gen.v78i4.713
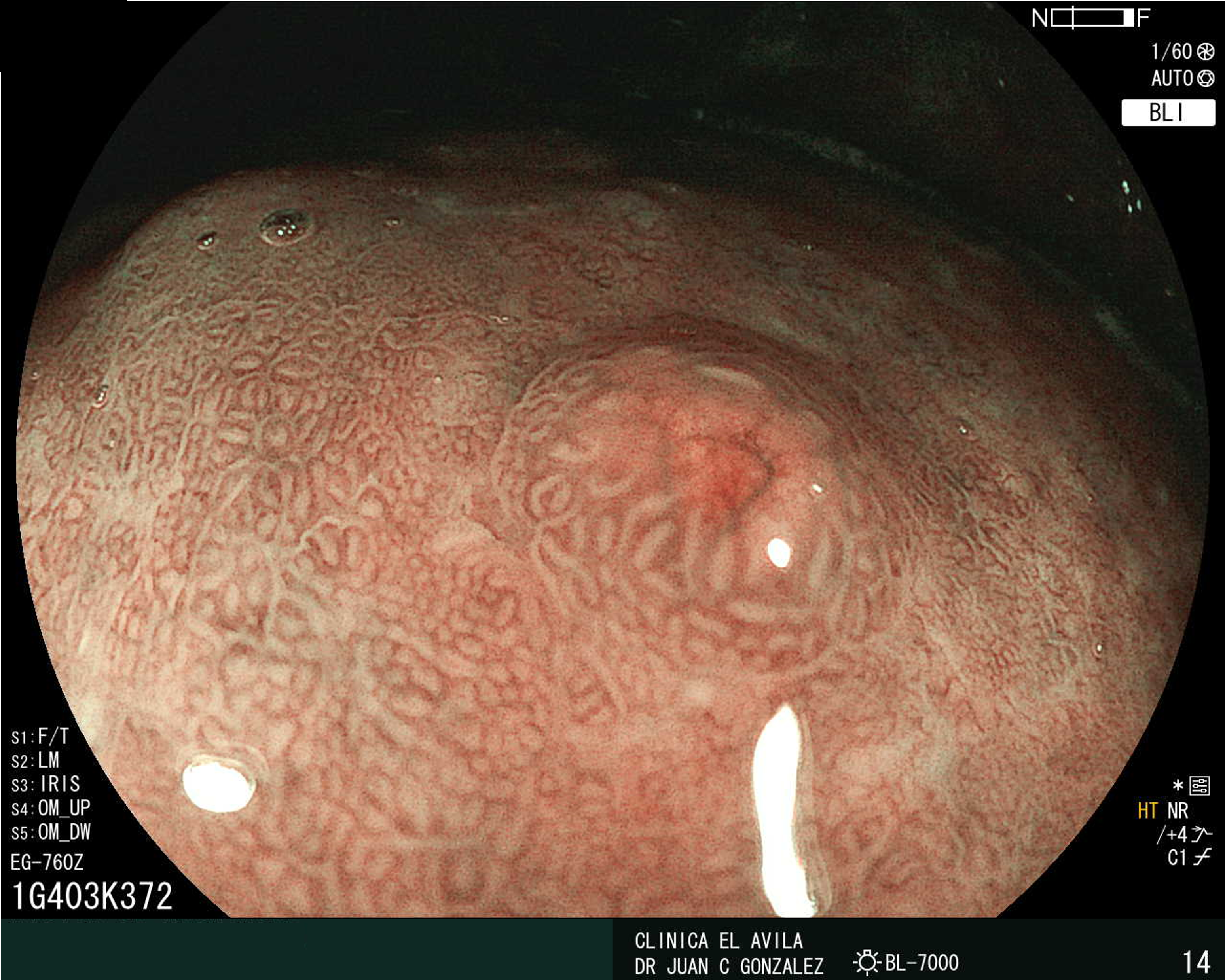
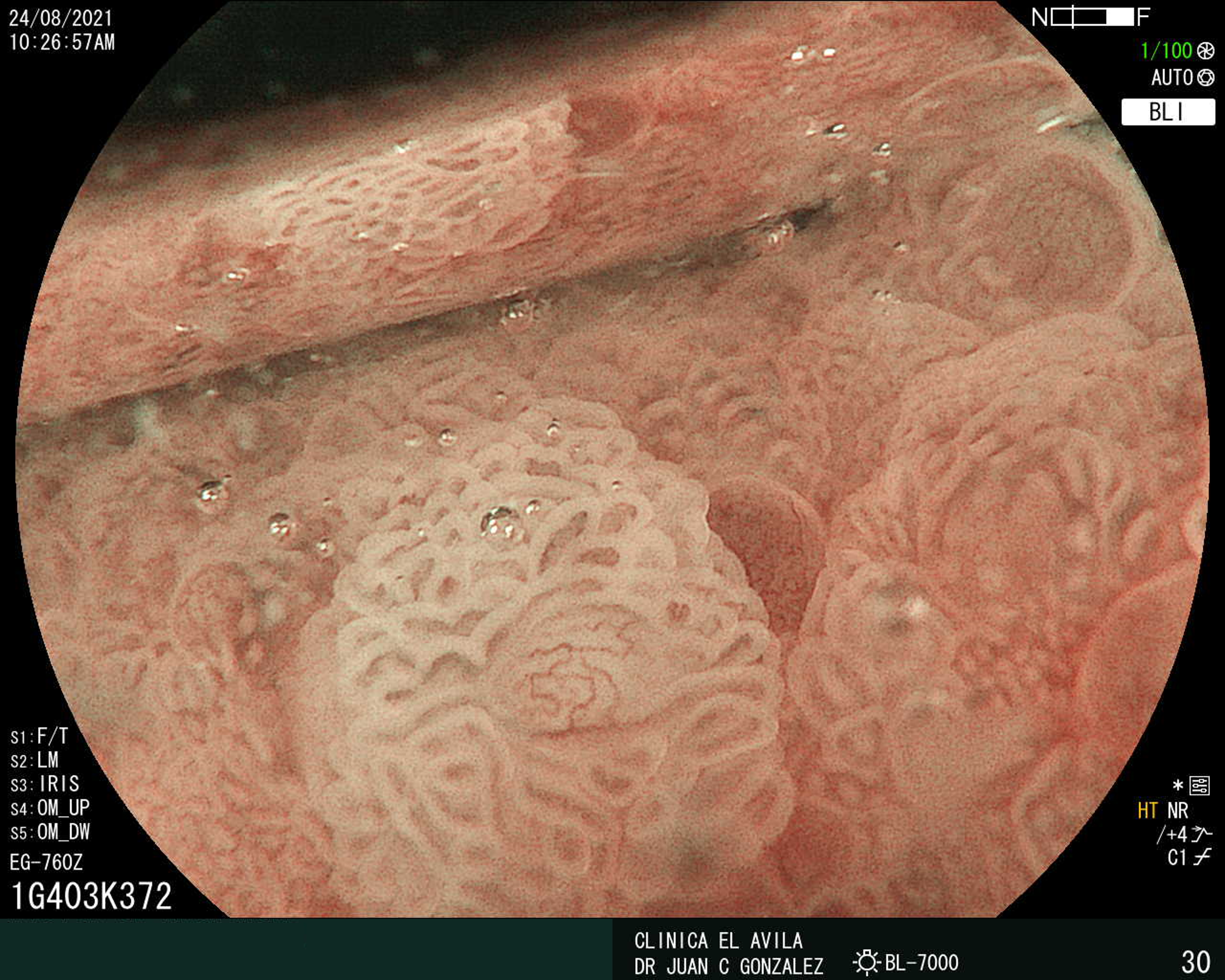
IMÁGENES GEN
| Figura 1. Tumor Neuroendocrino Gástrico | Figura 2. Hiperplasia de Células Neuroendocrinas en estómago |
 |  |
 |  |  |
ISSN: 0016-3503 e-ISSN: 2477-975X