Disbiosis en la microbiota intestinal
Resumen
Palabras clave
Texto completo:
PDFReferencias
Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E. Dysbiosis and the immune system Nat Rev Immunol. 2017;17(4):219-232. doi: 10.1038/nri.2017.7.
Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R. Diversity, stability and resilience of the human gut microbiota. Nature. 2012;489(7415):220-30. doi: 10.1038/nature11550.
Moreno-Calderón X, Vialva-Guerrero A, Núñez-Bello M, et al. Estudio observacional de la microbiota intestinal aeróbica. Kasmera. 2020;48(2): e48231547. doi: 10.5281/zenodo.4053038.
Borenstein E, Kupiec M, Feldman MW, Ruppin E. Large-scale reconstruction and phylogenetic analysis of metabolic environments. Proc Natl Acad Sci U S A. 2008;105(38):14482-7. doi: 10.1073/pnas.0806162105.
Freilich S, Kreimer A, Borenstein E, et al. Metabolic-network-driven analysis of bacterial ecological strategies. Genoma Biol. 2009;10(6): R61. doi: 10.1186/gb-2009-10-6-r615.
Stappenbeck TS, Virgen HW. Accounting for reciprocal host– microbiome interactions in experimental science. Nature. 2016 ;534(7606):191-9. doi: 10.1038/nature18285.
Thaiss CA, Itav S, Rothschild D, et al. Persistent microbiome alterations modulate the rate of post-dieting weight regain. Nature. 2016;540(7634):544-551. doi: 10.1038/nature20796.
Nagpal R, Mainali R, Ahmadi S, et al. Gut microbiome and aging: Physiological and mechanistic insights. Nutrition and Healthy Aging. 2018;4(4):267-285. Doi: 10.3233/NHA-170030.
Collado MC, Rautava S, Aakko J, Isolauri E, Salminen S. Human gut colonisation may be initiated in utero by distinct microbial communities in the placenta and amniotic fluid. Sci Rep. 2016; 6:23129. doi: 10.1038/srep23129.
Nagpal R, Tsuji H, Takahashi T, et al. Ontogenesis of the gut microbiota development in healthy fullterm vaginally-born breast-fed infants over the first 3 years of life: A quantitative bird’s-eye view. Front Microbiol. 2017; 8:1388. doi: 10.3389/fmicb.2017.01388.
Favier CF, Vaughan EE, De Vos WM, Akkermans AD. Molecular Monitoring of Succession of Bacterial Communities in Human Neonates. Appl Environ Microbiol. 2002;68(1):219-26. doi: 10.1128/AEM.68.1.219-226.2002.
Weiss GA, Hennet T. Mechanisms and consequences of intestinal dysbiosis Cell Mol Life Sci. 2017;74(16):2959-2977. doi: 10.1007/s00018-017-2509-x.
Tang WHW, Bäckhed F, Landmesser U, Hazen SL. Intestinal Microbiota in Cardiovascular Health and Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019 Abr 30;73(16):2089-2105. doi: 10.1016/j.jacc.2019.03.024.
Schmidt TSB, Raes J, Bork P. The Human Gut Microbiome: From Association to Modulation. Cell. 2018;172(6):1198-1215. doi: 10.1016/j.cell.2018.02.044.
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104(34):13780-5. doi: 10.1073/pnas.0706625104.
Garrett WS, Lord GM, Punit S, et al. Communicable ulcerative colitis induced by T-bet deficiency in the innate immune system. Cell. 2007;131(1):33-45. doi: 10.1016/j.cell.2007.08.017.
Buffington SA, Di Prisco GV, Auchtung TA, Ajami NJ, Petrosino JF, Costa-Mattioli M. Microbial Reconstitution Reverses Maternal Diet-Induced Social and Synaptic Deficits in Offspring. Cell. 2016;165(7):1762-1775. doi: 10.1016/j.cell.2016.06.001.
Hsiao EY, McBride SW, Hsien S, et al. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013;155(7):1451-63. doi: 10.1016/j.cell.2013.11.024.
Buffie CG, Bucci V, Stein RR, et al. Precision microbiome reconstitution restores bile acid mediated resistance to Clostridium difficile. Nature. 2015;517(7533):205-8. doi: 10.1038/nature13828.
Milani C, Duranti S, Bottacini F, et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol Mol Biol Rev. 2017;81(4): e00036-17. doi: 10.1128/MMBR.00036-17.
Sommer F, Anderson JM, Bharti R, Raes J, Rosenstiel P. The resilience of the intestinal microbiota influences health and disease. Nat Rev Microbiol. 2017;15(10):630-638. doi: 10.1038/nrmicro.2017.58.
Hall A, Tolonen A, Xavier R. Variación genética humana y el microbioma intestinal en la enfermedad. Nat Rev Genet. 2017,18: 690–699. https://doi.org/10.1038/nrg.2017.63.
Wang J, Thingholm LB, Skiecevičienė J, et al. Genome-wide association analysis identifies variation in vitamin D receptor and other host factors influencing the gut microbiota. Nat Genet. 2016 Nov;48(11):1396-1406. doi: 10.1038/ng.3695.
Putignani L, Del Chierico F, Petrucca A, Vernocchi P, Dallapiccola B. The human gut microbiota: a dynamic interplay with the host from birth to senescence settled during childhood. Pediatr Res. 2014;76(1):2-10. doi: 10.1038/pr.2014.49. Epub 2014 Abr 14. PMID: 24732106.
Mitchell EL, Davis AT, Brass K, et al. Reduced intestinal motility, mucosal barrier function, and inflammation in aged monkeys. J Nutr Health Aging. 2017;21(4):354-61.
Rea MC, O’Sullivan O, Shanahan F, et al. Clostridium difficile Carriage in Elderly Subjects and Associated Changes in the Intestinal Microbiota. J Clin Microbiol. 2011; 867-875. doi:10.1128/JCM.05176-11.
Thevaranjan N, Puchta A, Schulz C, et al. Age-Associated Microbial Dysbiosis Promotes Intestinal Permeability, Systemic Inflammation, and Macrophage Dysfunction. Cell Host Microbe. 2017;21(4):455-466.e4. doi: 10.1016/j.chom.2017.03.002.
Lupp C, Robertson ML, Wickham ME, et al. Host-mediated inflammation disrupts the intestinal microbiota and promotes the overgrowth of Enterobacteriaceae. Cell Host Microbe. 2007;2(2):119-29. doi: 10.1016/j.chom.2007.06.010.
Stecher B, Robbiani R, Walker AW, et al. Salmonella enterica Serovar Typhimurium Exploits Inflammation to Compete with the Intestinal Microbiota. PLoS Biol. 2007;5(10):2177-89. doi: 10.1371/journal.pbio.0050244.
Arthur JC, Perez-Chanona E, Mühlbauer M, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Ciencia. 2012;338(6103):120-3. doi: 10.1126/science.1224820.
Ayres JS, Trinidad NJ, Vance RE. Lethal inflammasome activation by a multidrug-resistant pathobiont upon antibiotic disruption of the microbiota. Nat. Med. 2012;18(5):799-806. DOI: 10.1038/nm.2729.
Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006; 12(12):1365-1371. doi: 10.1038/nm1511.
Duan H, Yu L, Tian F, Zhai Q, Fan L, Chen W. Antibiotic-induced gut dysbiosis and barrier disruption and the potential protective strategies. Crit Rev Food Sci Nutr. 2022;62(6):1427-1452. doi: 10.1080/10408398.2020.1843396.
Shi Y, Kellingray L, Zhai Q, et al. Structural and functional alterations in the microbial community and immunological consequences in a mouse model of antibiotic-induced dysbiosis. Frontiers in Microbiology. 2018; 9:1948. doi: 10.3389/fmicb.2018.01948.
Shi Y, Zhao X, Zhao J, et al. A mixture of Lactobacillus species isolated from traditional fermented foods promote recovery from antibiotic-induced intestinal disruption in mice. J App Microbiol. 2018; 124 (3):842–54. doi: 10.1111/jam.13687.
Shi Y, Zhai Q, Dongyao L, et al. Restoration of cefixime-induced gut microbiota changes by Lactobacillus cocktails and fructooligosaccharides in a mouse model. Microbiological Research. 2017; 200:14–24. doi: 10.1016/j.micres. 2017.04.001.
Sarah Larcombe, Melanie L. Hutton, Dena L. Involvement of Bacteria Other Than Clostridium difficile in Antibiotic-Associated Diarrhoea. Trends in Microbiol. 2016; 24(6): 463-476. doi: 10.1016/j.tim.2016.02.001.
Moreno X, Armas A, Panizo MM, Garcés MF. Formación de biopelículas por Klebsiella pneumoniae aislada en heces de pacientes con Trastorno del Espectro Autista. RVSM. 2019; 40:12-18. Disponible en: http://saber.ucv.ve/ojs/index.php/rev_vm/article/view/20382/0.
De Filippo C, Cavalieri D, Di Paola M, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107(33):14691-6. doi: 10.1073/pnas.1005963107.
Yatsunenko T, Rey FE, Manary MJ, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486(7402):222-7. doi: 10.1038/nature11053.
Song M, Chan AT, Sun J. Influence of the Gut Microbiome, Diet, and Environment on Risk of Colorectal Cancer. Gastroenterología. 2020;158(2):322-340. doi: 10.1053/j.gastro.2019.06.048.
O'Keefe SJ, Li JV, Lahti L, et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun. 2015; 6:6342. doi: 10.1038/ncomms7342.
Moszak M, Szulińska M, Bogdański P. You Are What You Eat—The Relationship between Diet, Microbiota, and Metabolic Disorders—A Review. Nutrients. 2020;12(4):1096. doi: 10.3390/nu12041096.
Zmora N, Suez J, Elinav E. You are what you eat: diet, health and the gut microbioma. Nat Rev Gastroenterol Hepatol. 2019; 16(1):35-56. doi: 10.1038/s41575-018-0061-2.
Icaza-Chávez ME. Microbiota intestinal en la salud y la enfermedad. Rev Gastroenterol México 2013;78(4):240–248. doi.org/10.1016/j.rgmx.2013.04.004
Radaic A, Kapila YL. El oraloma y su disbiosis: The oralome and its dysbiosis: New insights into oral microbiome-host interactions. Comput Struct Biotechnol J. 2021; 19:1335-1360. doi: 10.1016/j.csbj.2021.02.010.
Greenbaum S, Greenbaum G, Moran-Gilad J, Weintraub AY. Ecological dynamics of the vaginal microbiome in relation to health and disease. Am J Obstet Gynecol. 2019 Abr;220(4):324-335. doi: 10.1016/j.ajog.2018.11.1089.
Neugent ML, Hulyalkar NV, Nguyen VH, Zimmern PE, De Nisco NJ. Advances in Understanding the Human Urinary Microbiome and Its Potential Role in Urinary Tract Infection. mBio. 2020;11(2): e00218-20. doi: 10.1128/mBio.00218-20.
Houghteling PD, Walker WA. From birth to ‘immuno-health’, allergies and enterocolitis. J Clin Gastroenterol. 2015 Nov-Dic;49 Suppl 1(0 1):S7-S12. doi: 10.1097/MCG.00000000000000355.
Maiuolo J, Gliozzi M, Musolino V, et al. The Contribution of Gut Microbiota–Brain Axis in the Development of Brain Disorders Neurosci frontal. 2021; 15:616883. doi: 10.3389/fnins.2021.616883.
DOI: http://dx.doi.org/10.61155/gen.v76i1.602
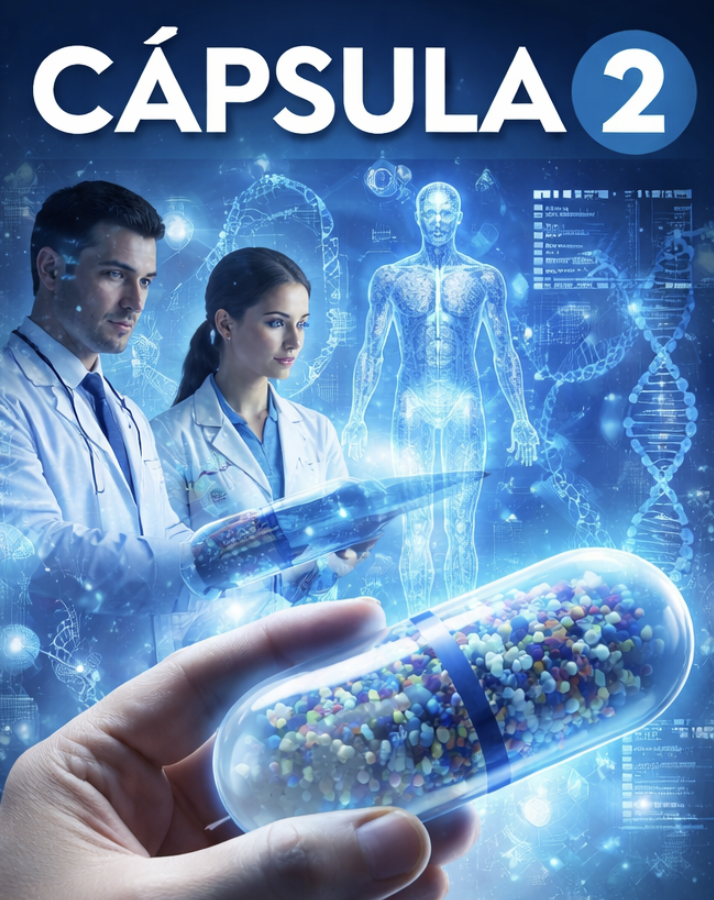
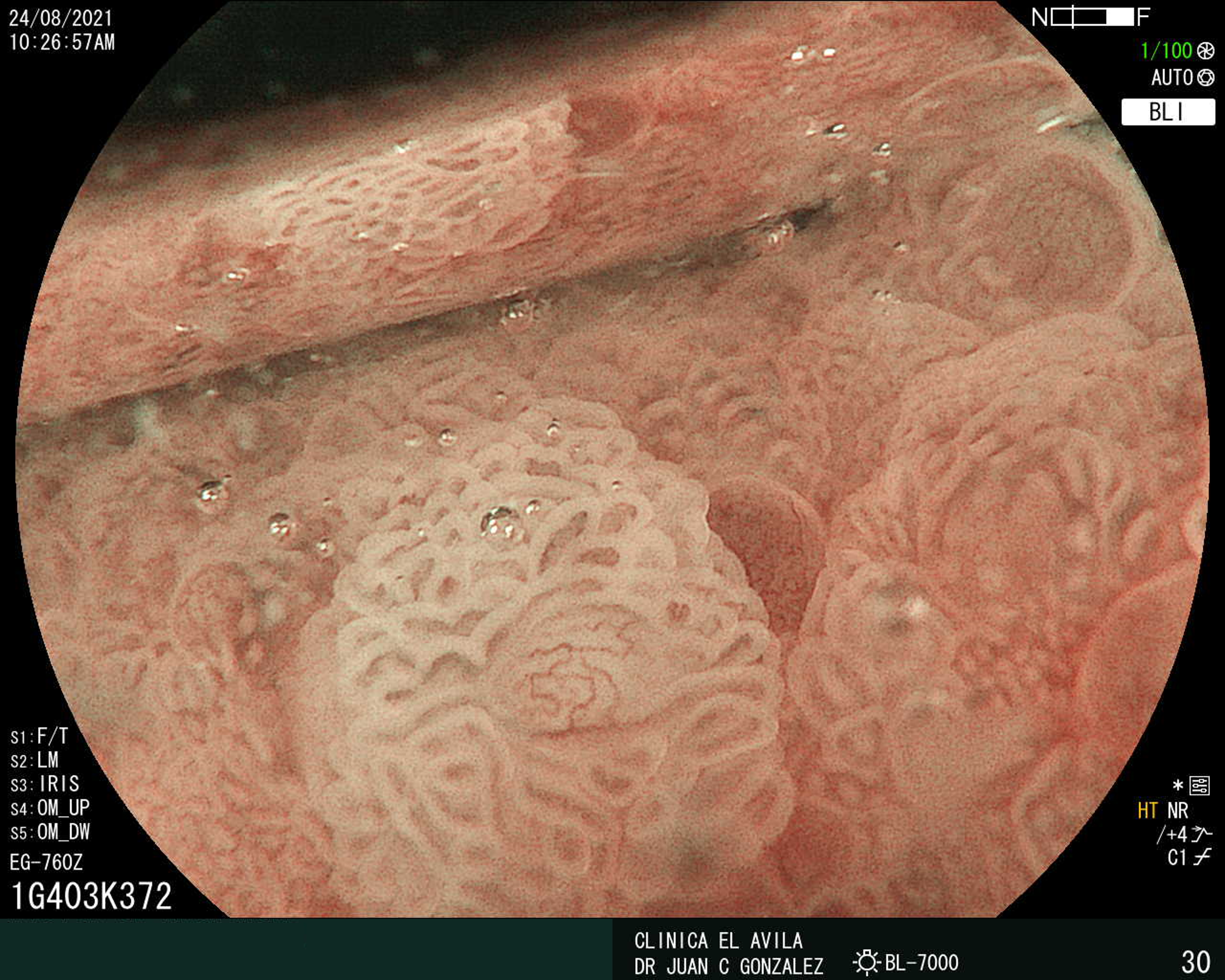
IMÁGENES GEN
| Figura 1. Tumor Neuroendocrino Gástrico | Figura 2. Hiperplasia de Células Neuroendocrinas en estómago |
 |  |
 |  |  |
ISSN: 0016-3503 e-ISSN: 2477-975X