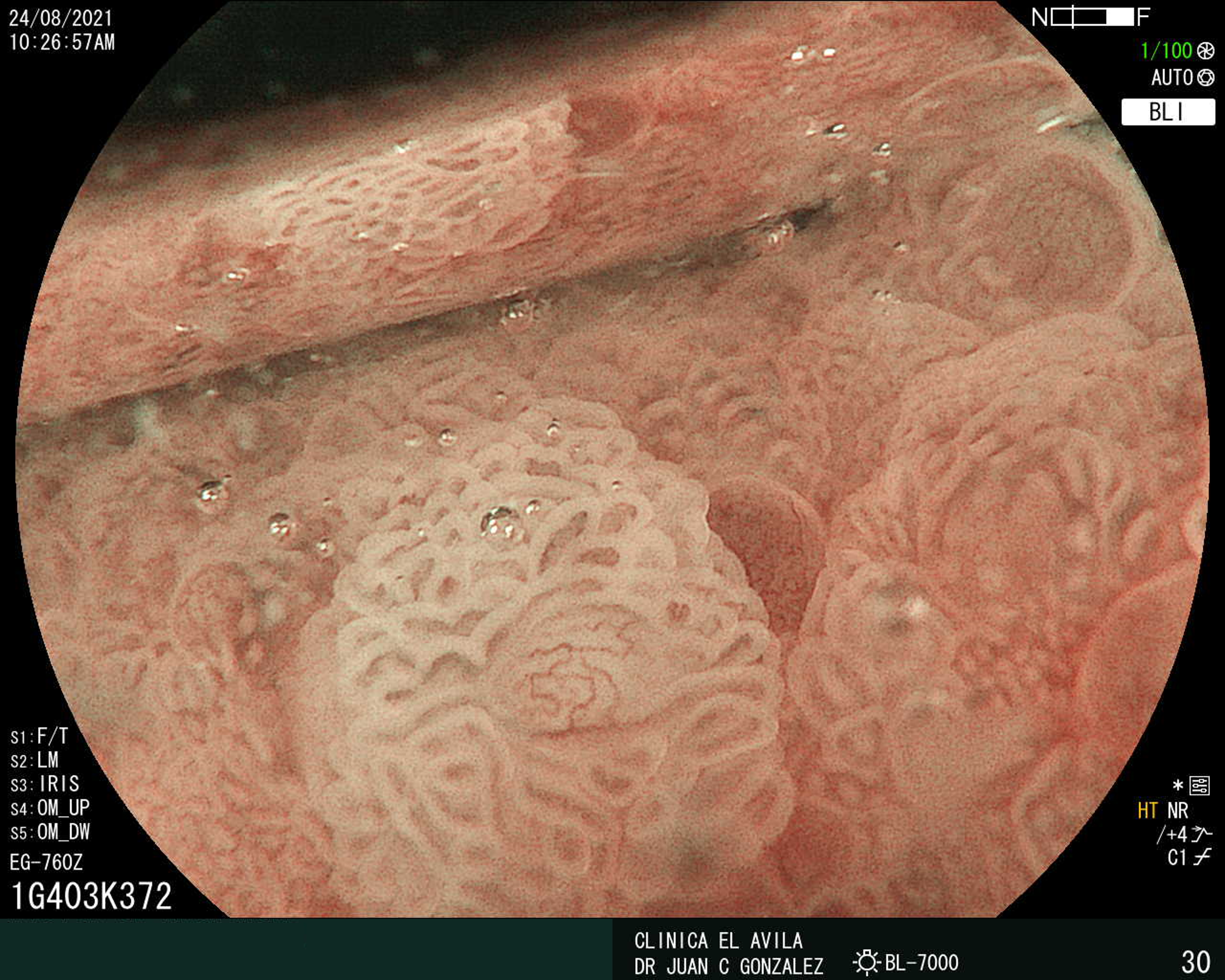
Cromoendoscopia virtual utilizando BLIen el diagnóstico endoscópico de esófago de Barrett neoplásico y no neoplásico
Resumen
Palabras clave
Texto completo:
PDFReferencias
-Jung KW, Talley NJ, Romero Y et al. Epidemiology and natural history of intestinal metaplasia of thegastroesophageal junction and Barrett's esophagus: a population-based study. Am J Gastroenterol 2011; 106:1447–1455. doi: 10.1038/ajg.2011.1302-Sampliner RE. Practice guidelineson the diagnosis, surveillance, and therapy of Barrett's esophagus. The Practice ParametersCommittee of the American College of Gastroenterology. Am J Gastroenterol. 1998; 93 (7): 1028-1032. doi: 10.1111/j.1572-0241.1998.003623-Spechler SJ, Sharma P, Souza R.F. et al. American Gastroenterological Association medical position statement on the management of Barrett's esophagus. Gastroenterology 2011; 140:1084-91. doi: 10.1053/j.gastro.2011.01.0304-Hur C, Miller M, Kong CY, et al. Trends in esophageal adenocarcinoma incidence and mortality. Cancer 2013; 119:1149-58. doi: 10.1002/cncr.278345-Fitzgerald RC, Di Pietro M, RagunathK, et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett's oesophagus. Gut. 2014; 63:7–42. doi: 10.1136/gutjnl-2013-3053726-6-Shaheen NJ, Falk GW, Iyer PG, et al. ACG Clinical Guideline: Diagnosis and Management of Barrett’s Esophagus. American Journal of Gastroenterolog. 2016;111(1):30-50. doi: 10.1038/ajg.2015.3227-Qumseya B, Sultan S, Bain P, et al. ASGE guideline on screening and surveillance of Barrett’s Esophagus. Gastrointestinal Endoscopy. 2019;90(3):339-359. doi: 10.1016/j.gie.2019.05.0128. Corley DA, Kubo AI, DeBoer J, et al. Diagnosing Barrett’s esophagus: reliability of clinical and pathologic diagnoses. Gastrointest Endosc. 2009 May; 69(6): 1004–1010. doi: 10.1016/j.gie.2008.07.0359. Cjalasani N, Wo JM, Hunter JG, et al. Significance of intestinal metaplasia in different areas of esophagus including esophagogastric junction Dig Dis Sci 1997; 42:603-607. doi: 10.1023/a:101886352977710-Sharma P, McQuaid K, Dent J, et al. A critical review of the diagnosis and management of Barrett’s esophagus: the AGA Chicago workshop. Gastroenterology 2004; 127:310–30. doi: 10.1053/j.gastro.2004.04.01011-11-Kariv R, Plesec TP, Goldblum JR, et al. The Seattle protocol does not more reliably predict the detection of cancer at the time of esophagectomy than a less intensive surveillance protocol. Clin Gastroenterol Hepatol 2009; 7:653–8. doi: 10.1016/j.cgh.2008.11.02412 -Abrams JA, Kapel RC, Lindberg GM, et al. Adherence to biopsy guidelines for Barrett’s esophagus surveillance in the community setting in the United States. Clin Gastroenterol Hepatol 2009; 7:736–42. doi: 10.1016/j.cgh.2008.12.02713-Sampliner RE Updated guidelines for the diagnosis, surveillance, and therapy of Barrett's esophagus. Am J Gastroenterol. 2002; 97(8):1888-1895. doi: 10.1111/j.1572-0241.2002. 05910.x
-Woolf GM, Riddell RH, Robert H, et al. Gastroeintestinal Endoscopy 1989; 35:541-544. DOI: 10.1016/s0016-5107(89)72907-2. doi: 10.1016/s0016-5107(89)72907-215-Canto MI, Setrakian S, Petras R, et al. Gastrointestinal Endoscopy 1996; 44:1-7. DOI: 10.1016/s0016-5107(96)70221-3. doi: 10.1016/s0016-5107(96)70221-316 . Canto MI, Setrakian S, Willis J, et al. Gastrointestinal Endoscopy 2000:51:560-568. doi: 10.1016/s0016-5107(00)70290-217-Reyes AA. Nuevas técnicas de imagen (iSCAN, NBI, FICE). Rev Gastroenterol Mex. 2011;76 Supl 1:134-136.18-Silva FB, Dinis-Ribeiro M, Vieth M, et al. Endoscopic assessment and grading of Barrett’s esophagus using magnification endoscopy and narrow-band imaging: Accuracy and interobserver agreement of different classification systems. Gastrointest Endosc. 2011; 73:7–14. doi: 10.1016/j.gie.2010.09.023 19-. Qumseya BJ, Wang H, Badie N, et al. Advanced imaging technologies increase detection of dysplasia and neoplasia in patients with barrett’s esophagus: A meta-analysis and systematic review. Clinical Gastroenterology and Hepatology. 2013.Dec;11(12):1562-70. doi: 10.1016/j.cgh.2013.06.01720-Subramanian V, Ragunath K, Hirchowitz BI, et al. Advanced endoscopic imaging: a review of commercially available technologies. Clin Gastroenterol Hepatol. 2014;12(3):368–76. doi: 10.1016/j.cgh.2013.06.01521. Sano Y, Kobayashi M, Hamamoto Y, et al. New diagnostic method based on color imaging using narrow band imaging (NBI) system for gastrointestinal tract. DDW Atlanta 2001 [abstract]: A696. 22. Gono K, Yamaguchi M, Ohyama N. Improvement of image quality of the electroendoscopy by narrowing spectral shapes of observation light. In: Imaging Society of Japan. Proceedings of International Congress Imaging Science, May 13-17, Tokyo, Japan: Imaging Society of Japan, 2002: 399-400.23. 23-Shinya K, Fujishiro M. Novel image-enhanced endoscopy with i-scan technology. World Journal of Gastroenterology, 2010; 16(9): 1043-1049. doi: 10.3748/wjg. v16.i9.104324. Gono K, Oby T, Yamaguchi M, et al. Appearance of enhanced tissue features in narrow band endoscopic imaging. Journal of Biomedical Optic 2004; 9(3):568-577. doi: 10.1117/1.169556325-Miyake Y KT, Takeuchi S, Tsumura N, et al. Development of new electronic endoscopes using the spectral images of an internal organ. In: Proceedings of the IS&T/SID’s Thirteen Color Imaging Conference, 2005. Scottsdale, Ariz; 2005. 261-269.26. Osawa H, Yamamoto H. Present and future status of flexible spectral imaging co or enhancement and blue laser imaging technology. Dig Endosc. 2014 Jan; 26 Suppl 1:105-15. doi: 10.1111/den.12205l27.Osawa H, Miura Y, Takezawa T, et al. Linked color images and blue laser for the detection of the upper gastrointestinal tract. Clin Endosc 2018; 51: 513-526. doi: 10.5946/ce.2018.13228. ASGE Technology Committee; Thosani N, Abu Dayyeh BK, Sharma P, et al. ASGE Technology Committee systematic review and metaanalysis assessing the ASGE Preservation and Incorporation of Valuable Endoscopic Innovations thresholds for adopting real-time imaging-assisted endoscopic targeted biopsy during endoscopic surveillance of Barrett’s esophagus. Gastrointest Endosc 2016; 83:684-98. doi: 10.1016/j.gie.2016.01.00729. Subramaniam S, Kandiah K, Schoon E, et al. Development and validation of the international blue-light imaging for Barrett's neoplasia classification. Gastrointestinal Endoscopy.2022;91(2): 310-320. doi: 10.1016/j.gie.2019.09.03530. Singh R, Anagnostopoulos GK, Yao K, et al. Narrow-band imaging with magnification in Barrett’s esophagus: Validation of a simplified grading system of mucosal morphology patterns against histology. Endoscopy. 2008; 40:457–63. doi: 10.1055/s-2007-99574131. Kara MA, Ennahachi M, Fockens P, et al. Detection and classification of the mucosal and vascular patterns (mucosal morphology) in Barrett’s esophagus by using narrow band imaging. Gastrointest Endosc. 2006; 64(2):155-166. doi: 10.1016/j.gie.2005.11.049 32. Sharma P, Bansal A, Mathur S, et al. The utility of a novel narrow band imaging endoscopy system in patients with Barrett’s esophagus. Gastrointest Endosc. 2006; 64:167–75. doi: 10.1016/j.gie.2005.10.04433. Baldaque-Silva F, Marques M, Lunet N, et al. Endoscopic assessment and grading of Barrett’s esophagus using magnification endoscopy and narrow band imaging: Impact of structured learning and experience on the accuracy of the Amsterdam classification system. Scand J Gastroenterol.2013;48:160–167.doi:10.3109/00365521.2012.74639234.Lipman G, Bisschops R, Sehgal V, et al. Systematic assessment with I-SCAN magnification endoscopy and acetic acid improves dysplasia detection in patients with Barrett’s esophagus. Endoscopy. 2017; 49:1219–1228. doi: 10.1055/s-0043-11344136. González JC, Ruiz ME. Atlas de Imágenes Endoscópicas FICE. Editorial Versilia. 2009.37. González JC, Dos Reis V. Esófago de Barrett y Cromoscópia Electronica. Gen 2016;70(3):71-75.38. González JC, Del Monte R. Atlas de Imágenes Endoscópicas BLI/LCI. Editorial Bell-Tech. 2020.39. Goldblum JR. Controversies in the diagnosis of Barrett esophagus and Barrett-related dysplasia: one pathologist's perspective. Arch Pathol Lab Med. 2010; 134:1479-1484. doi: 10.5858/2010-0249-RA.1
Duits L, Phoa KN, Curvers WL, et al. Barrett's oesophagus patients with low-grade dysplasia can be accurately risk-stratified after histological review by an expert pathology panel. Gut.2015;64(5):700-706. doi: 10.1136/gutjnl-2014-30727841. Prashanth V, Vijay K, John G, et al. Discordance Among Pathologists in the United States and Europe in Diagnosis of Low-grade Dysplasia for Patients WithBarrett's Esophagus. Gastroenterology. 2017;152(3):564-570. doi: 10.1053/j.gastro.2016.10.041
DOI: http://dx.doi.org/10.61155/gen.v77i4.463
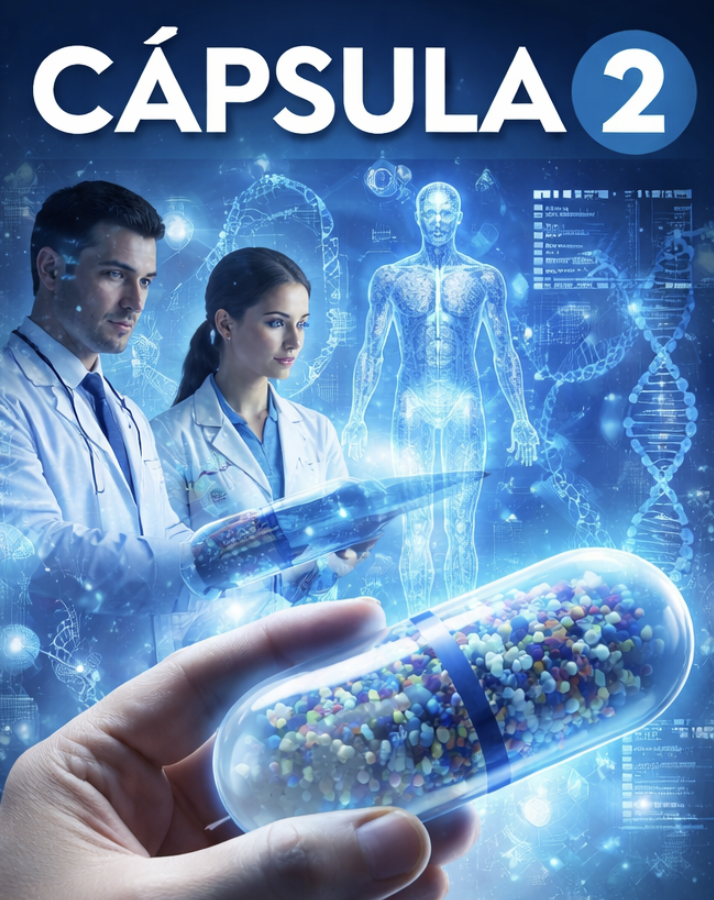
IMÁGENES GEN
| Figura 1. Tumor Neuroendocrino Gástrico | Figura 2. Hiperplasia de Células Neuroendocrinas en estómago |
 |  |
 |  |  |
ISSN: 0016-3503 e-ISSN: 2477-975X