Cáncer de páncreas
Resumen
Palabras clave
Texto completo:
PDFReferencias
GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2019; 4: 934–47.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman H, McCain R. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 2018; 24(43): 4846-4861.
Somashekar G, Li F, Bhattacharya A, Ladha H, Porter K, Singh A, et al. Differentiation of pancreatic ductal adenocarcinoma from other neoplastic solid pancreatic lesions: a tertiary oncology center experience. Gastrointest Endosc. 2015;81:370-9.
Eloubeidi MA, Decker GA, Chandrasekhara V, Chathadi KV, Early DS, Evans JA, et al. ASGE guidelines. The role of endoscopy in the evaluation and management of patients with solid pancreatic neoplasia. Gastrointest Endosc 2016;83 (1):17-27.
Lee L, Andersen D, Ashida R, Brugge W, Canto M, Chang K, et al. EUS and related technologies for the diagnosis and treatment of pancreatic disease: research gaps and opportunities Summary of a National Institute of Diabetes and Digestive and Kidney Diseases workshop. Gastrointest Endosc 2017;86:768-78.
Bang J, Navaneethan U, Hasan M, Hawes R, Varadarajulu S. Stent placement by EUS or ERCP for primary biliary decompression in pancreatic cancer: a randomized trial. Gastrointest Endosc 2018;88:9-17.
Ferlay J, Colombet L, Soerjomataram I, Mathers C, Parkin M, Piñeros M. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Clinical Trial Service Unit & Epidemiological Studies Unit, University of Oxford, Oxford, U.K.
Caglevic C. at el. Recomendaciones sobre el manejo del cáncer de páncreas tipo adenocarcinoma en Latinoamérica. Reunión del Consenso del Simposio Latinoamericano de Gastroenterología Oncológica (SLAGO) y de la Asociación Ibero Latinoamericana de Terapia Radiante (ALATRO). Revista medica de Chile 144(10):1305-1318.
Lopez P. Martinez L. Cáncer de páncreas. Epidemiología de su mal pronóstico. Rev Méd Urug 2017; 33(3):122-128.
Ilic M. Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol 2016 November 28; 22(44): 9694-9705.
Zhang Q., Zeng L.,Chen L., et al. Pancreatic Cancer Epidemiology, Detection, and Management. Gastroenterol Res and Pract Volume 2016, Article ID 8962321.
DaVee T., Coronel E., Papafragkakis C., Thaiudom S., Lanke G., Chakinala R. at el. Pancreatic cancer screening in high-risk individuals with germline genetic mutations. Gastrointest Endosc 2018;87:1443-50.
Bruno M. Pancreatic cancer screening in high-risk individuals: Ready for prime time?. Gastrointest Endosc 2018;86:1452-53.
Maisonneuve P, Lowenfels A. Risk factors for pancreatic cancer: a summary review of meta-analytical studies. Inter Journal of Epidem;2015, 186–198.
Iodice S, Gandini S, Maisonneuve P, Lowenfels AB. Tobacco and the risk of pancreatic cancer: a review and meta-analysis. Langenbecks Arch Surg 2008; 393: 535-545.
Tramacere I, Scotti L, JenabM et al. Alcohol drinking and pancreatic cancer risk: a meta-analysis of the dose-risk relation. Int J Cancer 2010;126:1474–86.
Brewer O. & Lennon A. Chronic pancreatitis-like changes in individuals at high risk for the development of pancreatic cancer: What is the significance?. Gastrointest Endosc 2019;89:852-53.
Raimondi S., Lowenfels A., Morselli-Labate A., Maisonneuve P., Pezzilli R. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best Pract Res Clin Gastroenterol 2010; 24: 349-358.
Thiruvengadam S., Chuang J., Huang R., Girotra M., Park W.Chronic pancreatitis changes in high-risk individuals for pancreatic ductal adenocarcinoma. Gastrointest Endosc 2019;89:842-51.
Xu M., Jung X., Hines J., Eibl G., & Chen Y. Obesity and Pancreatic Cancer: Overview of Epidemiology and Potential Prevention by Weight Loss. Pancreas. 2018; 47(2):158–162.
Li D, Morris JS, Liu J, et al. Body mass index and risk, age of onset, and survival in patients with pancreatic cancer. JAMA. 2009; 301:2553–2562.
Kasenda B, Bass A, Koeberle D, et al Surival in overweight patients with advanced pancreatic carcinoma: a multicentre cohort study. BMC Cancer. 2014; 14:728.
Wang F., Herrington M., Larsson J., Permert J. Review The relationship between diabetes and pancreatic cancer. Molecular Cancer 2003, 2:1-4.
Huxley R, Ansary-Moghaddam A, Berrington de González A, Barzi F, Woodward M. Type-II diabetes and pancreatic cancer: a meta-analysis of 36 studies. British Journal of Cancer 2005; 92: 2076-2083.
Paluszkiewicz P, Smolin´ ska K, De˛bin´ ska I., et al. Main dietary compounds and pancreatic cancer risk. The quantitative analysis of case-control and cohort studies. Cancer Epidemiol 2012;36:60–67.
Genkinger JM, Li R, Spiegelman D et al. Coffee, tea, and sugarsweetened carbonated soft drink intake and pancreatic cancer risk: a pooled analysis of 14 cohort studies. Cancer Epidemiol Biomarkers Prev 2012;21:305–18.
Wahi MM, Shah N, Schrock CE, Rosemurgy AS 2nd, Goldin SB. Reproductive factors and risk of pancreatic cancer in women: a review of the literature. Ann Epidemiol 2009; 19: 103-111.
Wolpin B., Kraft P., Gross M., Helzlsouer K., & col. Pancreatic cancer risk and ABO blood group alleles: results from the pancreatic cancer cohort consortium. Cancer Res 2010; 70: 1015-1023.
Guertin K., Freedman N., Loftfield E., Stolzenberg R., Graubard B. & Sinha R. A prospective study of coffee intake and pancreatic cancer: results from the NIH-AARP Diet and Health Study. British J Cancer 2015;113:1081–85.
Chen F., Roberts N., Klein A. Inherited pancreatic cancer. Chinise Clin Oncol 2017; 6: 58.
Chiaro M., Segersvärd R., Lohr M., Verbeke C. Early detection and prevention of pancreatic cancer: is it really possible today? World J Gastroenterol 2014; 20: 12118-1213.
Grover S., Syngal S. Hereditary pancreatic cancer. Gastroenterology 2010;139:1076–80.
Klein A., Brune K., Petersen G., et al. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res 2004;64:2634-8.
Riva G., Pea A., Pilati C., Fiadone G., et al. Histo-molecular oncogenesis of pancreatic cancer: From precancerous lesions to invasive ductal adenocarcinoma. World J Gastrointest Oncol 2018 October 15; 10(10): 317-27.
Malagelada J., et al. Lesiones quísticas pancreáticas. Libro: Directrices mundiales de la WGO Lesiones quísticas pancreáticas. 4-25.
Ferreira R., Sancho R.,. Messal h., et al. Duct- and Acinar-Derived Pancreatic Ductal Adenocarcinomas Show Distinct Tumor Progression and Marker Expression. Cell Reports 2017, 21:966–978.
Pusateri A.,& Krishna S. Review Pancreatic Cystic Lesions: Pathogenesis and Malignant Potential. Diseases 2018; 6(50):2-12
D’Angelica M., Brennan, M., Suriawinata A., Klimstra D., Conlon K. Intraductal Papillary Mucinous Neoplasms of the Pancreas. Ann. Surg. 2004;239:400–8.
Grutzmann R., Niedergethmann M.,Pilarsky C., Kloppel G., Saeger H. Intraductal papillary mucinous tumors of the pancreas: Biology, diagnosis, and treatment. Oncologist 2010; 15:1294–309.
Kobayashi M, Fujinaga Y, Ota H. Reappraisal of the Immunophenotype of Pancreatic Intraductal Papillary Mucinous Neoplasms (IPMNs)-Gastric Pyloric and Small Intestinal Immunophenotype Expression in Gastric and Intestinal Type IPMNs-. Acta Histochem Cytochem 2014; 47: 45-57.
Moriya T, Kimura W, Semba S, Sakurai F, Hirai I, Ma J, Fuse A, Maeda K, Yamakawa M. Biological similarities and differences between pancreatic intraepithelial neoplasias and intraductal papillary mucinous neoplasms. Int J Gastrointest Cancer 2005; 35: 111-19.
Lin F., Chen Z., Wang H.Utility of Immunohistochemistry in the Pancreatobiliary Tract. Arch Pathol Lab Med. 2015;139:24–38.
Tanaka M., Fernandez-del Castillo C., Kamisawa T., et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 2017; 17:738¬-53.
Levink I., Bruno M., Cahen D. Management of Intraductal Papillary Mucinous Neoplasms: Controversies in Guidelines and Future Perspectives. Curr Treat Options Gastro 2018; 16:316–32.
Keane MG, Horsfall L, Rait G, Pereira SP. A case-control study comparing the incidence of early symptoms in pancreatic and biliary tract cancer. BMJ Open 2014; 4: e005720.
Hippisley-Cox J, Coupland C. Identifying patients with suspected pancreatic cancer in primary care: derivation and validation of an algorithm. Br J Gen Pract 2012;62:e38–45.
Stapley S, Peters TJ, Neal RD, et al. The risk of pancreatic cancer in symptomatic patients in primary care: a large case-control study using electronic records. Br J Cancer 2012;106:1940–4.
Kim JE, Lee KT, Lee JK, Paik SW, Rhee JC, Choi KW. Clinical usefulness of carbohydrate antigen 19-9 as a screening test for pancreatic cancer in an asymptomatic population. J Gastroenterol Hepatol 2004; 19: 182-186.
Jans J., Talma M., almonacid M., cruz J., et al. Rendimiento diagnóstico del marcador tumoral ca 19-9 en la diferenciación entre patología bilio-pancreática benigna y maligna. Rev chil cir. Agosto 2013; 65(4):307-14.
Fahrmann J., Bantis L., Capello M., Scelo G., Dennison J., et al. A Plasma-Derived Protein-Metabolite Multiplexed Panel for Early-Stage Pancreatic Cancer. J Natl Cancer Inst 2018;111(4):372-379.
Ashida R., Tanaka S., Yamanaka H., Okagaki S., at el. Review The Role of Transabdominal Ultrasound in the Diagnosis of Early Stage Pancreatic Cancer: Review and Single-Center Experience. Diagnostics 2019;9:2-9.
Sun E., & Min J. Imaging diagnosis of pancreatic cancer: A state-of-the-art review. World J Gastroenterol 2014; 20(24): 7864-77.
Kanno, A., Masamune, A., Hanada, K., Maguchi, H., et al. Multicenter study of early pancreatic cancer in Japan. Pancreatology 2018, 18, 61–67.
Martínez A., D’Onofrio M. Ultrasonography of the pancreas. 1. Conventional imaging. Abdom Imaging 2007; 32: 136-49.
Granata V., Fusco R., Catalano O., Sergio Venanzio S., at el. Multidetector computer tomography in the pancreatic adenocarcinoma assessment: an update. Infectious Agents and Cancer (2016) 11:57.
Buchsa N., Frossardb J., Rossetc A., Chilcotta M., at el. Vascular invasion in pancreatic cancer. SWISS MED WKLY 2007;137:286–291.
Wang X., Yang F., Jin C., & Fu D. Utility of PET/CT in diagnosis, staging, assessment of resectability and metabolic response of pancreatic cancer. World J Gastroenterol 2014 November 14; 20(42): 15580-89.
Gerritsen A., Bollen T., Nio Y., Molenaar Q., at el. Diagnostic value of a pancreatic mass on computed tomography in patients undergoing pancreatoduodenectomy for presumed pancreatic cancer. Surgery 2015;158:173-82.
Eloubeidi M., Decker A., Chandrasekhara V., at el. The role of endoscopy in the evaluation and management of patients with solid pancreatic neoplasia. Gastrointest Endosc 2016;83(1):17-28.
Bronstein Y., Loyer E., Kaur H., & col. Detection of small pancreatic tumors with multiphasic helical CT. AJR Am J Roentgenol 2004;182: 619-23.
Muller M., Meyenberger C., Bertschinger P., at el. Pancreatic tumors: evaluation with endoscopic US, CT, and MR imaging. Radiology 1994;190:745-51.
DeWitt J., Devereaux B., Chriswell M., et al. Comparison of endoscopic ultrasonography and multidetector computed tomography for detecting and staging pancreatic cancer. Ann Intern Med 2004;141: 753-63.
Gress F., Hawes R., Savides T., at el. Role of EUS in the preoperative staging of pancreatic cancer: a large single-center experience. Gastrointest Endosc 1999;50:786-91.
Oh H., Kang H., Lee J., & col. Diagnostic accuracy of 22/25-gauge core needle in endoscopic ultrasound-guided sampling: systematic review and meta-analysis. Korean J Intern Med 2016;31:1073-83.
Hirooka Y., Itoh A., Kawashima H., at el. Diagnosis of pancreatic disorders using contrast-enhanced endoscopic ultrasonography and endoscopic elastography. Clin Gastroenterol Hepatol 2009;7(suppl):S63-7.
Mei M, Ni J, Liu D, et al. EUS elastography for diagnosis of solid pancreatic masses: a meta-analysis. Gastrointest Endosc 2013;77:578-89.
Gill K., & Wallace M. EUS elastography for pancreatic mass lesions: between imageand FNA?. Gastrointest Endosc 2008;68(5):1095-97.
Chantarojanasiri T., y Kongkam P. Endoscopic ultrasound elastography for solid pancreatic Lesions. World J Gastrointest Endosc 2017 October 16; 9(10): 506-13.
Jafri M., Sachdev A., Khanna L., & Gress F. The Role of Real Time Endoscopic Ultrasound Guided Elastography for Targeting EUS-FNA of Suspicious Pancreatic Masses: A Review of the Literature and A Single Center Experience. J Pancreas 2016 Sep 08;17(5):516-24.
Dietrich CF, Saftoiu A, Jenssen C. Real time elastography endoscopic ultrasound (RTE-EUS), a comprehensive review. Eur J Radiol 2014; 83:405-14.
Iglesias-García J.; et al. Endoscopic ultrasound enhancement elastography Gastrointest Endosc Clin N Am. 2012; 70(6):1101-08.
Iglesias-García J., et al.. Quantitative Endoscopic Ultrasound Elastography: An Accurate Method for the Differentiation of Solid Pancreatic Masses. Gastroenterology October 2010;139(4):1172-80.
Săftoiu A., Vilmann P., Gorunescu F., Janssen J., Hocke M., Larsen M., Iglesias-Garcia J., et al. European EUS Elastography Multicentric Study Group. Accuracy of endoscopic ultrasound elastography used for differential diagnosis of focal pancreatic masses: a multicenter study. Endoscopy 2011; 43: 596-603.
Giovannini M, Hookey LC, Bories E, et al. Endoscopic Ultrasound Elastography: the First Step towards Virtual Biopsy? Preliminary Results in 49 patients. Endoscopy 2006; 38: 344-48.
Giovannini M., Botelberge T., Bories E., Pesenti C., et al. Endoscopic ultrasound elastography for evaluation of lymph nodes and pancreatic masses: A multicenter study. World J Gastroenterol 2009 April 7; 15(13): 1587-93.
Carrara S., Di Leo M., Grizzi F., Correale L., et al. EUS elastography (strain ratio) and fractal-based quantitative analysis for the diagnosis of solid pancreatic lesions. Gastrointest Endosc 2018;87:1464-73.
Dawwas MF, Taha H, Leeds JS, Nayar MK, Oppong KW. Diagnostic accuracy of quantitative EUS elastography for discriminating malignant from benign solid pancreatic masses: a prospective, single-center study. Gastrointest Endosc 2012;76:953-61.
Kongkam P., Lakananurak N., Navicharern P., Chantarojanasiri T., et al. Combination of EUS-FNA and elastography (strain ratio) to exclude malignant solid pancreatic lesions: A prospective single-blinded study. J Gastroenterol Hepatol 2015; 30: 1683-89.
Okasha H., Elkholy S., El-Sayed R., Wifi M., et al. Real time endoscopic ultrasound elastography and strain ratio in the diagnosis of solid pancreatic lesions. World J Gastroenterol. 2017 Aug 28;23(32):5962-68.
Okasha H., Mahdy R., Elkholy S., Hassan M., at el. Endoscopic ultrasound (EUS) elastography and strain ratio, could it help in differentiating malignant from benign pancreatic lesions?. Medicine (Baltimore). 2018 Sep;97(36):e11689.
Fusaroli P., Napoleon B., Gincul R., Lefort C., et al. The clinical impact of ultrasound contrast agents in EUS: a systematic review according to the levels of evidence. Gastrointest Endosc 2016;84:587-96.
Fusaroli P., SPADA A., GRAZIA M., & CALETTI G. Contrast Harmonic Echo–Endoscopic Ultrasound Improves Accuracy inDiagnosis of Solid Pancreatic Masses. Clinical gastro and hepat 2010;8:629–34.
Napoleon B., Alvarez M., Gincoul R., Pujol B., et al. Contrast-enhanced harmonic endoscopic ultrasound in solid lesions of the pancreas: results of a pilot study. Endoscopy. 2010; 42:564–70.
Lee T., Cheon Y., Shim C. Clinical role of contrast-enhanced harmonic endoscopic ultrasound in differentiating solid lesions of the pancreas: a single-center experience in Korea. Gut Liver. 2013; 7:599–604.
Park J., Kim H., Bang B., Kim S., Jeong S., Lee D. Effectiveness of contrast-enhanced harmonic endoscopic ultrasound for the evaluation of solid pancreatic masses. World J Gastroenterol. 2014; 20:518–24.
Gincul R., Palazzo M., Pujol B., Tubach F., Palazzo L., et al. Contrast-harmonic endoscopic ultrasound for the diagnosis of pancreatic adenocarcinoma: a prospective multicenter trial. Endoscopy. 2014; 46:373–379.
Saftoiu A., Vilmann P., Dietrich C., Iglesias-Garcia J., et al. Quantitative contrast-enhanced harmonic EUS in differential diagnosis of focal pancreatic masses (with videos). Gastrointest Endosc. 2015; 82:59–69.
Keun M., Moon S., Jun T., Kim R., at el. Contrast-Enhanced Endoscopic Ultrasound for Differentially Diagnosing Autoimmune Pancreatitis and Pancreatic Cancer. Gut Liver 2018.
He X., Ding Y., Sun L. Contrast-enhanced endoscopic ultrasound for differential diagnosis of pancreatic cancer: an updated meta-analysis. Oncotarget 2017; 8(39): 66392-401.
Mei S., Wang M., Sun L. Contrast-Enhanced EUS for Differential Diagnosis of Pancreatic Masses: A Meta-Analysis. Gastroenterology Research and Practice 2019, 2019, Arti.1670183,1-9.
Saftoiu A., Peter Vilmann P., Bhutani M. The role of contrast‑enhanced endoscopic ultrasound in pancreatic adenocarcinoma. Endoscopic ultrasound 2016; 5(6):368-72.
Yamashita Y., Shimokawa T., Napoleo B., Pietro f., et al. Value of contrast‑enhanced harmonic endoscopic ultrasonography with enhancement pattern for diagnosis of pancreatic cancer: A meta‑analysis. Digest Endosc 2019; 31(2):125-33.
Chung Y., Kim K. Contrast-enhanced ultrasonography: advance and current status in abdominal imaging. Ultrasonography 2015;34:3-18.
Facciorusso A., Wani S., Triantafyllou K., et al. Comparative accuracy of needle sizes and designs for EUS tissue sampling of solid pancreatic masses: a network meta-analysis. Gastrointest Endosc 2019;90:893-903.
Kitano M., Yoshida T., Itonaga M., Tamura T., et al. Impact of endoscopic ultrasonography on diagnosis of pancreatic cancer. J Gastroenterol 2019; 54:19–32.
Yoshida T., Yamashita Y., Kitano M. Endoscopic Ultrasound for Early Diagnosis of Pancreatic Cancer. Diagnostics 2019; 9(81):2-8.
Seicean A., Badea R., Moldovan-Pop A., Vultur S., Botan E., et al. Harmonic Contrast-Enhanced Endoscopic Ultrasonography for the Guidance of Fine-Needle Aspiration in Solid Pancreatic Masses. Ultraschall Med. 2017 Apr;38(2):174-182.
Nakai Y., Takahara N., Mizuno S., Kogure H., Koike K. Current Status of Endoscopic Ultrasound Techniques for Pancreatic Neoplasms. Clin Endosc 2019;52:527-32.
Nawaz H, Fan CY, Kloke J, et al. Performance characteristics of endoscopic ultrasound in the staging of pancreatic cancer: a meta-analysis. JOP 2013;14:484-97.
Montejo L., Rios A., Sarrria O., et al. Staging pancreatic carcinoma by computed tomography. Radiolog 2018;60(1):10-23.
Allen, P. J. et al. Multi-institutional Validation Study of the American Joint Commission on Cancer (8th Edition) Changes for T and N Staging in Patients With Pancreatic Adenocarcinoma. Ann Surg 2017;265:185–191.
Demir I., Jäger C., Schlitter A., Konukiewitz B., Stecher L., et al. R0 Versus R1 Resection Matters after Pancreaticoduodenectomy, and Less after Distal or Total Pancreatectomy for Pancreatic Cancer. Ann Surg 2 2018;268(6):1058-68.
Kim KS, Kwon J, Kim K, Chie EK. Impact of Resection Margin Distance on Survival of Pancreatic Cancer: A Systematic Review and Meta-Analysis. Cancer Res Treat 2017; 49: 824-833.
Gaag N., Rauws E., Eijck C., et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 2010;362:129‑37.
Tol J., Hooft J., Timmer R., et al. Metal or plastic stents for preoperative biliary drainage in resectable pancreatic cancer. British Journal of Cancer 2016;65:1981‑7.
Domínguez J.,Lariño J.,Iglesias j. Biliary drainage in pancreatic cancer: The endoscopic retrograde cholangiopancreatography perspective. Endoscopic Ultrasound 2017; 6(3):117-121.
Neoptolemos J., Stocken D., Bassi C., Ghaneh P., et al. Europea Study Group for Pancreatic Cancer. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA 2010; 304: 1073-81.
Neoptolemos J., Palmer D., Ghaneh P., Psarelli E., Valle J., et al. European Study Group for Pancreatic Cancer. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet 2017; 389: 1011-24.
Mahaseth H., Brutcher E., Kauh J., Hawk N., et al. Modified FOLFIRINOX regimen with improved safety and maintained efficacy in pancreatic adenocarcinoma. Pancreas 2013; 42: 1311-15.
Levy M., Alberts S., Bamlet W., Burch P., et al. EUS-guided fine-needle injection of gemcitabine for locally advanced and metastatic pancreatic cancer. Gastrointest Endosc 2017;86:161-9.
Di Matteo F., Saccomandi P., Martino M., Pandolfi M., & col. Feasibility of EUS-guided Nd:YAG laser ablation of unresectable pancreatic adenocarcinoma. Gastrointest Endosc 2018;88(1):168-74.
Crino S., D’Onofrio M., Bernardoni L., et al. EUS-guided Radiofrequency Ablation (EUS-RFA) of Solid Pancreatic Neoplasm Using an 18-gauge Needle Electrode: Feasibility, Safety, and Technical Success. J Gastrointestin Liver Dis 2018; 27(1): 67-72.
Coronel E., Cazacu I., Sakuraba A., et al. EUS-guided fiducial placement for GI malignancies: a systematic review and meta-analysis. Gastrointest Endosc 2019;89:659-70.
Gardner T., Spangler C.,. Byanova K., at el. Cost-effectiveness and clinical efficacy of biliary stents in patients undergoing neoadjuvant therapy for pancreatic adenocarcinoma in a randomized controlled trial. Gastrointest Endosc 2016;84:460-6.
Seo D., Sherman S., Dua K., Slivka A., et al. Covered and uncovered biliary metal stents provide similar relief of biliary obstruction during neoadjuvant therapy in pancreatic cancer: a randomized trial. Gastrointest Endosc 2019;90:602-12.
Waldthaler A., Rutkowski W., Valente R., et al. Palliative therapy in pancreatic cancer interventional treatment with stents. Transl Gastroenterol Hepatol 2019;4:7.
Ardengh J, Lopes C, Kemp R, Dos Santos JS. Different options of endosonography-guided biliary drainage after endoscopic retrograde cholangio-pancreatography failure. World J Gastrointest Endosc 2018;10:99-10
Khan MA, Akbar A, Baron TH, Khan S, Kocak M, Alastal Y, et al. Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-Analysis. Dig Dis Sci 2016;61:684-703.
Perez-Miranda M, Tyberg A, Poletto D, Toscano E, Gaidhane M, Desai AP, et al.. EUS guided Gastrojejunostomy Versus Laparoscopic Gastrojejunostomy: An International Collaborative Study. J Clin Gastroenterol 2017;51:896-9.
Khashab MA, Bukhari M, Baron TH, Nieto J, El Zein M, Chen YI, et al. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open 2017;5:275-81.
DOI: http://dx.doi.org/10.61155/gen.v74i1.507
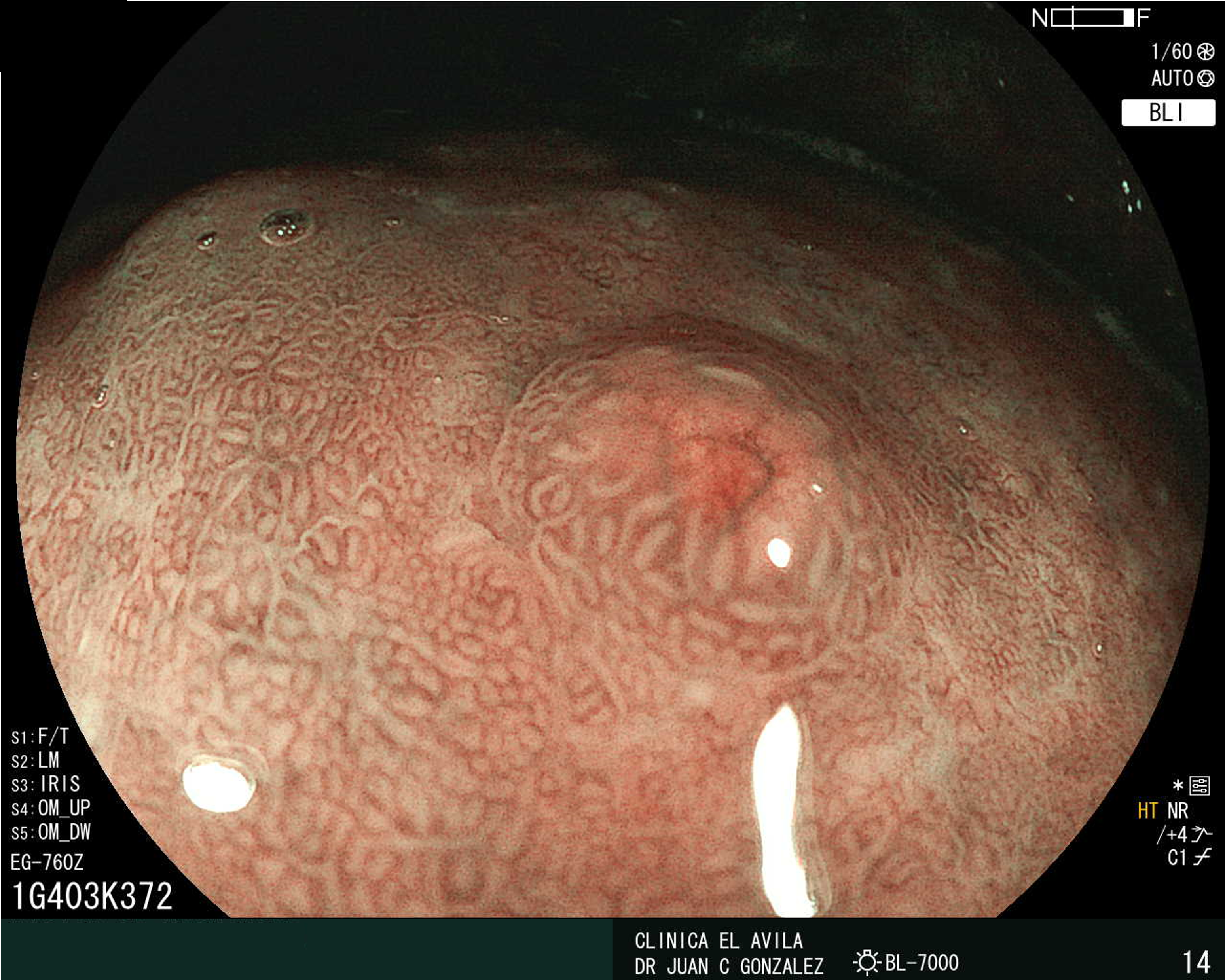
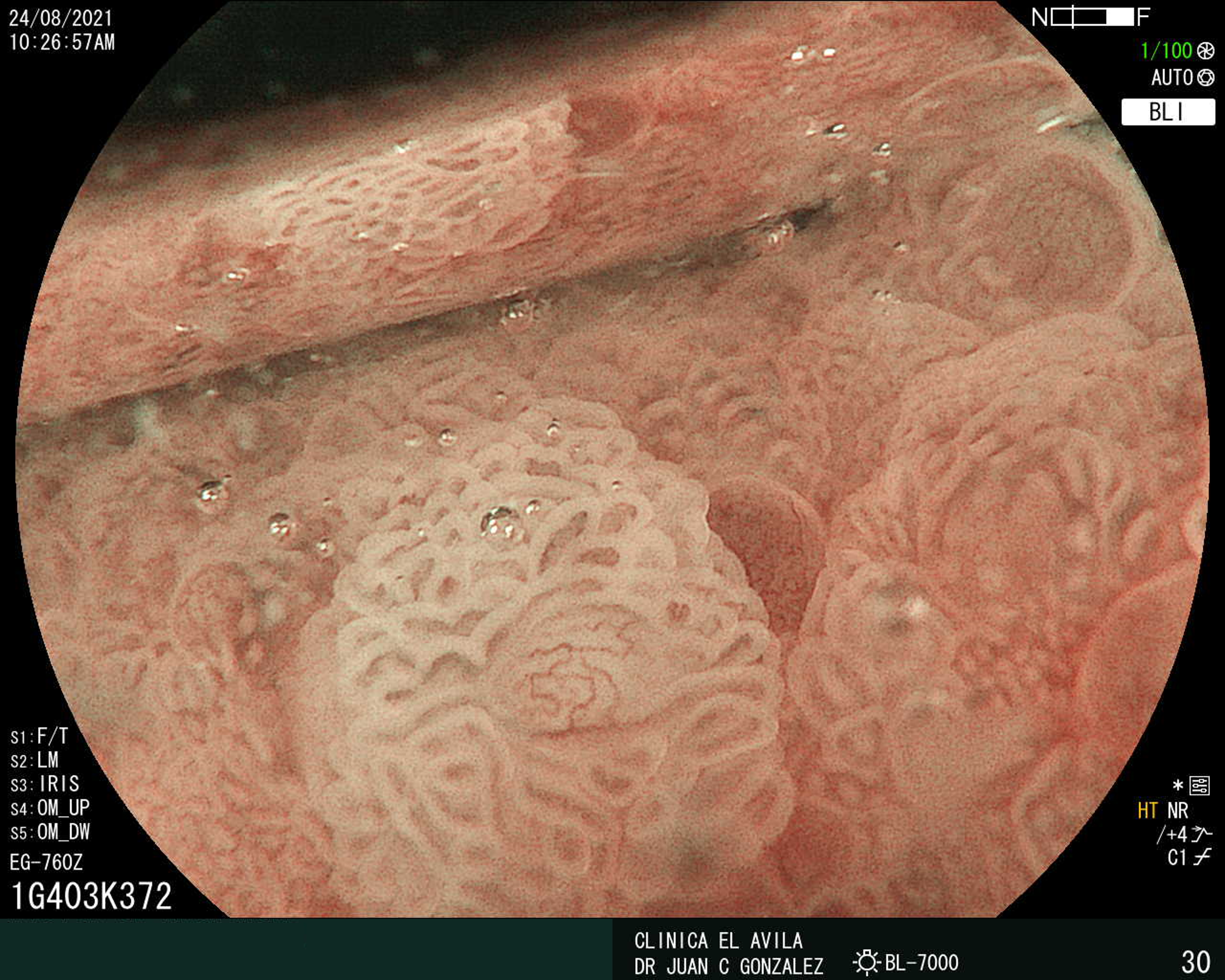
IMÁGENES GEN
| Figura 1. Tumor Neuroendocrino Gástrico | Figura 2. Hiperplasia de Células Neuroendocrinas en estómago |
 |  |
 |  |  |
ISSN: 0016-3503 e-ISSN: 2477-975X