Cirugía Bariátrica. Cambios fisiológicos en el tratamiento del Sindrome Metabólico
Resumen
El Síndrome metabólico (SM) se define por la presencia de 3 de 5 criterios clínicos: 1.Circunferencia abdominal ≥ 102cm en hombres u 88cm en mujeres 2. Triacilglicéridos (TAG) ≥150mg/dl 3. Lipoproteína de alta densidad (HDL) colesterol < 40 mg/dl en Hombres o 50 mg/dl en mujeres 4. Presión arterial ≥ 130/85 mmHg 5. Glicemia > 110 mg/dl. Se asocia a mayor riesgo de enfermedad cardiovascular, Diabetes Mellitus tipo 2 (DM2), Hipertensión Arterial (HTA) y daño a órganos blanco, como riñón. La cirugía bariátrica (CB) consiste en una serie de procedimientos quirúrgicos los cuales se clasifican de acuerdo la técnica empleada: técnicas restrictivas, malabsortivas y mixtas, cuyo objetivo principal es producir una pérdida de peso, al menos 50%, en un año y que se sostenga a largo plazo, produciendo múltiples efectos metabólicos beneficiosos para el organismo del paciente con sindrome metabólico.
Palabras clave
Texto completo:
PDFReferencias
Edith-Lopez M, Sosa M, Labrousse N. Sindrome metabólico. Revista de Posgrado de la VIa Cátedra de Medicina. 2007; 174: 12-15.
Lizarzaburu Robles J. Sindrome metabolico: concepto y aplicación practica. An Fac med. 2013; 74: 315-320.
Vandevijvere S, Chow C, Hall K, Umali E, Swinburn B Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull World Health Organ 2015; 93:446–456
Papaprito K. Cirugía para la obesidad: efectos generales, beneficios y riesgos. REV. MED. CLIN. CONDES 2012; 23: 189-195.
Sarwer D, Wadden T, Fabricatore A. Psychosocial and behavioral aspects of bariatric surgery. Obes. Res. 2005; 13: 639-648.
Solis-Ayala E, Carrillo-Ocampo L, Canche-Arenas A, Cortázar-Benítez L, Cabrera-Jardínez R, Rodriguez-Weber F, Diaz-Greene E. Cirugía bariátrica: resultados metabólicos y complicaciones. Med Int Mex 2013; 29: 487-494.
Csendes A, Papapietro K, Burgos A, Lanzarini E, Canobra M. Efecto del bypass gástrico a largo plazo (7 a 10 años) en pacientes con obesidad severa y mórbida sobre el peso corporal, diabetes, dislipidemia y desarrollo de anemia. Rev Med Chile 2011; 139: 1414-1420
Yupanqui H, Muñoz J, Guerra L. Obesidad y cirugía bariatrica: complicaciones clinicametabolicas. Acta Medica Colombiana 2008; 33: 15-21.
Maluenda F. Cirugia bariatrica. REV. MED. CLIN. CONDES 2012; 23: 180-188
Brethauer S, Chand B, Schauer P. Risks and benefits of bariatric surgery: Current evidence. Cleve Clin J Med 2006; 73: 993-1007.
Carcamo C. Cirugia de la obesidad morbida. Cuad. Cir. 2003; 17: 64-70
Musleh M, Carrillo K, Braghetto I. Restrictive bariatric surgery techniques:
Xanthakos S. Nutritional Deficiencies in Obesity and After Bariatric Surgery Pediatr Clin North Am. 2010; 56: 1-16
Ma I, Madura J. Gastrointestinal Complications After Bariatric Surgery. Clin Gastroenterol hepatol 2015; 11: 526-535.
Lujan J, Parilla P. Selección del paciente candidato a cirugía bariátrica y preparación preoperatoria. Cir Esp 2004; 75: 232-235
Fujioka K. Follow-up of nutritional and metabolic problems after bariatric surgery. Diabetes Care 2005; 28: 481-484.
Abeen G, Le Roux CW. Mechanism Underlying the Weight Loss and Complications of Roux-en-Y Gastric Bypass. Review. OBES SURG DOI 2015; s11695-015-1945-7
Ionut V, Burch M, Youdim A, Bergman R. Gastrointestinal hormones and bariatric surgery-induced weight loss. Obesity 2013; 21: 1093-1103
Corcelles R, Daigle C, Schauer P. MANAGEMENT OF ENDOCRINE DISEASE: Metabolic effects of bariatric surgery. Eur J Endocrinol 2016; 174: R19-R28.
Korner J, Bessler M, Cirilio L, Conwell I, Daud A, Restuccia N, Wardlaw S. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab 2005; 90: 359-365
Vincent R, Le Roux C. Changes in gut hormones after bariatric surgery. Clinical Endocrinology 2008; 69: 173-179
Laferrere B, Heshka S, Wang K, Khan Y, Mcginty J, Teixeira J, Hart A, Olivan B. Incretin Levels and Effect Are Markedly Enhanced 1 Month After Roux-en-Y Gastric Bypass Surgery in Obese Patients With Type 2 Diabetes. Diabetes Care 2007; 30: 1709-1716.
Christian-Heinz A, Tura A, Promintzer-Schifferl M, Prager G, Stadler M, Ludvik B, Esterbauer H, Bischof M, Luger A, Pacini G, Krebs M. Alterations in gastrointestinal, endocrine, and metabolic processes after bariatric Roux-en-Y gastric bypass surgery. Diabetes Care 2012; 35: 2580-2587.
Cummings D. Endocrine mechanisms mediating remission of diabetes after gastric bypass surgery. Int J Obes 2009; S33-S40.
Gupta A, Miegueu P, Lapointe M, Poirier P, Martin J, Bastien M, Tiwari S, Cianflone K. Acute post-bariatric surgery increase in orexin levels associates with preferential lipid profile improvement. PloS ONE 2014; 9: 1-8
Cummings D, Weigle D, Scott R, Breen P, Ma M, Dellinger E, Purnell J. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002; 346: 1623-1630.
Arterburn D, McCulloch D. Bariatric Surgery for Type 2 Diabetes: Getting Closer to the Long-term Goal. JAMA 2015; 150: 931-940 .
Dimova R, Tankova T. The Role of Vaspin in the Development of Metabolic and Glucose Tolerance Disorders and Atherosclerosis. BioMed Res. Int. 2015; 2015: 1-7
Lu H, Fouejeu P, Lapointe M, Poirier P, Martin J, Bastien M, Cianflone K. Increased Vaspin Levels Are Associated with Beneficial Metabolic Outcome Pre- and Post-Bariatric Surgery. PLOS ONE 2014; 9: e111002.
Ahmed M, Byrne C. Bariatric surgery and renal function: A precarious balance between benefit and harm. Nephrol Dial Transplant 2010; 25: 3142-3147
Heneghan H, Cetin D, Navaneethan S, Orzech N, Brethauer S, Schauer. Effects of bariatric surgery on diabetic nephropathy after 5 years of follow-up. Surg Obes Relat Dis 2013; 9: 7-14
Navarro-Diaz M, Serra A, Romero R, Bonet J, Bayés B, Homs M, Pérez N, Bonal J. Effect of drastic weight loss after bariatric surgery on renal parameters in extremely obese patients: long-term follow-up. J Am Soc Nephrol 2006; 17: S213-S217
Sharma S, McCauley J, Cottam D, Mattar S, Holover S, Dallal R, Lord J, Danner O, Ramanathan R, Eid G, Schauer P. Acute changes in renal function after laparoscopic gastric surgery for morbid obesity. Surg Obes Relat Dis 2006; 2: 389-392.
Poirier P, Cornier M, Mazzone T, Stiles S, Cummings S, Klein S, McCullough P, Fielding C, Franklin B. Bariatric Surgery and Cardiovascular Risk Factors: A Scientific Statement From the American Heart Association. Circulation 2011; 123: 1683-1701.
Romeo S, Maglio C. Cardiovascular events after bariatric surgery in obese subjects with type 2 diabetes. Diabetes Care 2012; 35: 2613-2617
Al Khalifa K, Al Ansari A, Alsayed A, Claudio V. The impact of sleeve gastrectomy on hyperlipidemia: a systematic review. J Obes 2013; 2013: 1-7
Abbatini F, Rizzello M, Casella G et al. Long-term effects oflaparoscopic sleeve gastrectomy, gastric bypass, and adjustable gastric banding on type 2 diabetes. Surg Endosc 2010; 24: 1005–1010.
Atkins E ,Preen D, Jarman C, Cohen L. Improved obesity reduction and co-morbidity resolution in patients treated with 40-french bougie versus 50-french bougie four years after laparoscopic sleeve gastrectomy. Analysis of 294 patients. Obes Surg 2012; 22: 97–104.
Benaiges D, Goday A, Ramon J, Hernandez E, Pera M, Cano J. Laparoscopic sleeve gastrectomy and laparoscopic gastric bypass are equally effective for reduction of cardiovascular risk in severely obese patients at one year of follow-up. Surg Obes Relat Dis 2011; 7: 575–580.
Benaiges D, Flores-Le-Roux J, Pedro-Botet J et al. Impact of restrictive (Sleeve Gastrectomy) vs hybrid bariatric surgery (Roux-en-Y Gastric Bypass) on lipid profile. Obes Surg 2012; 22: 1268–1275.
Boza C, Salinas J, Salgado N et al. Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1,000 cases and 3-year follow-up. Obes Surg 2012; 22: 866–871.
Chowbey P, Dhawan K, Khullar R et al. Laparoscopic sleeve gastrectomy: an indian experience-surgical technique and early results. Obes Surg 2010; 20: 1340–1347.
Hady H, Golaszewaski P, Zbucki R et al. The influence of laparoscopic adjustable gastric banding and laparoscopic sleeve gastectomy on weight loss, plasma ghrelin, insulin, glucose and lipids. Folia Hiosto Chemica 2012; 50: 292–303.
Hutter M, Schirmer B, Jones D et al. First report from the American College of Surgeons Bariatric Surgery CenterNetwork: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann. Surg, 2011; 254: 410–422.
Kehagias I, Karamanakos S, Argentou M, Kalfarentzos F. Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI<50 kg/m2. Obes Surg 2011; 21:1650–1656.
Lakdawala M, Bhasker A, Mulchandani D, Goel S, Jain S. Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic roux-en-y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg 2010; 20: 1–6.
Leivonen M, Juuti A, Jaser N, Mustonen H. Laparoscopic sleeve gastrectomy in patients over 59 years: early recovery and 12-month follow-up. Obes Surg 2011; 21: 1180–1187.
Nienhuijs S, Zoete J, Berende C, Hingh I, Smulders J. Evaluation of laparoscopic sleeve gastrectomy on weight loss and co-morbidity. Int J Surg 2010; 8: 302–304.
Omana J, Nguyen S,Herron D, Kini S. Comparison of comorbidity resolution and improvement between laparoscopic sleeve gastrectomy and laparoscopic adjustable gastric banding. Surg Endosc 2010; 24: 2513–2517.
González M, Lugli Z. Control personal de la conducta y Manga Gástrica. Revista de la Facultad de Medicina UCV, 2012; 35(1): 21-28.
Prasad P, Tantia O, Patle N, Khanna S, Sen B. An analysis of 1–3-year Follow-up results of laparoscopic sleeve gastrectomy: an indian perspective. Obes Surg 2012; 22: 507–514.
Ramalingamand G, Anton S. Our 1-year experience in laparoscopic sleeve gastrectomy. Obes Surg, 2011; 21:1828–1833.
DOI: http://dx.doi.org/10.61155/gen.v70i3.152
IMÁGENES GEN
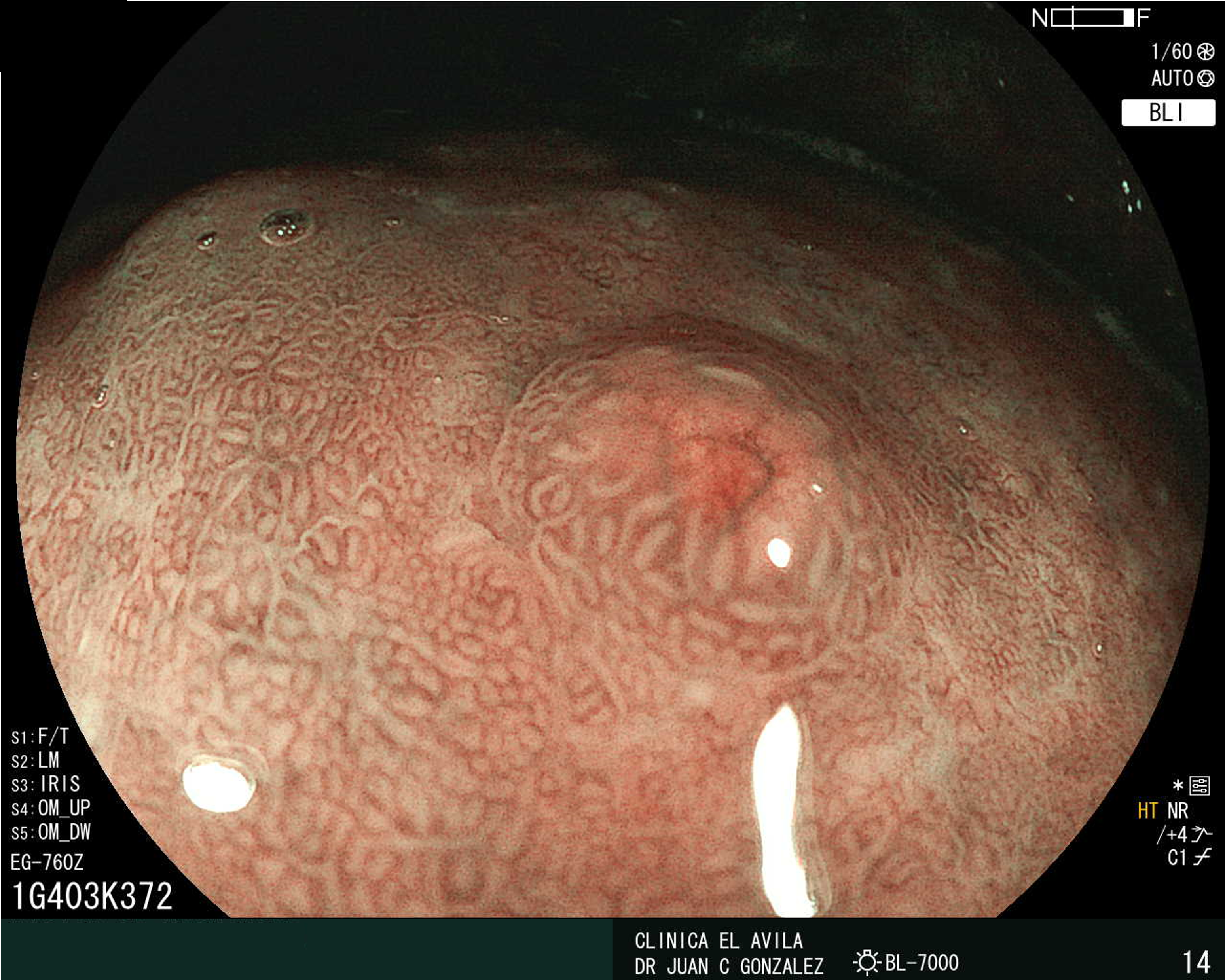
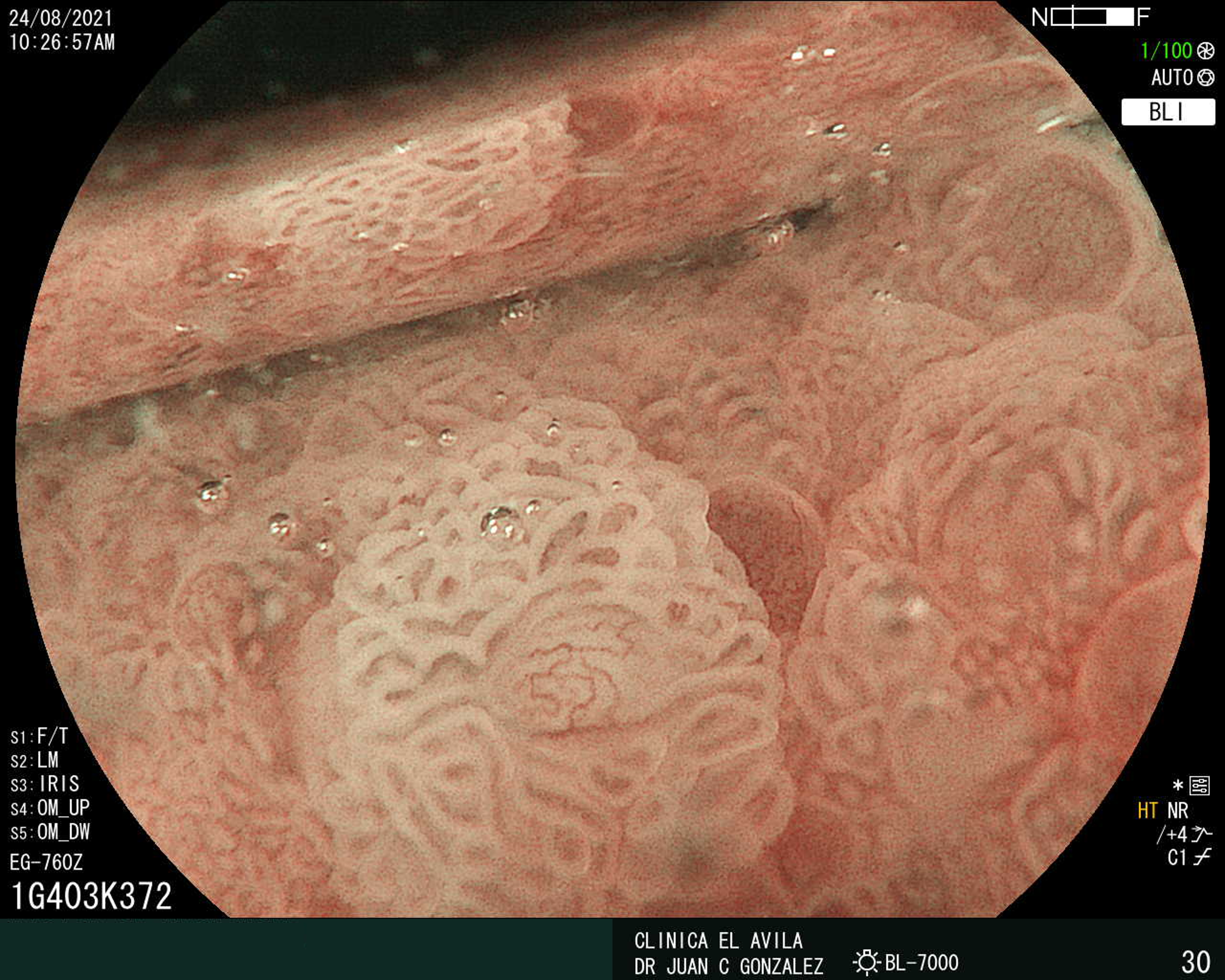
| Figura 1. Tumor Neuroendocrino Gástrico | Figura 2. Hiperplasia de Células Neuroendocrinas en estómago |
 |  |
 |  |  |
ISSN: 0016-3503 e-ISSN: 2477-975X








 ESCUCHAR RESUMEN DEL ARTICULO
ESCUCHAR RESUMEN DEL ARTICULO